Hashimoto's the cause of hypothyoid.
June 18, 2016
Hashimoto's is the most common cause of low thyroid or hypothyroid. In the Twin Cities of Minnesota, most low thyroid (hypothyroid) patients have Hashimoto's. Hashimoto's thyroiditis is an autoimmune condition that attack the thyroid. The medical treatment of Hashimoto's is to give replacement hormones (Levothyroxine or Synthroid). This rarely helps much, because nothing is being done for the autoimmune problem. In fact most patients in the Twin Cities of Minnesota are not even tested for it, even though most doctors know that Hashimoto's is the cause of low thyroid. Why is that you may ask? It is because there is no good drug for autoimmune attack on your thyroid. At LifeSpring Wellnes Center in Bloomington, Minnesota we test our patients for Hashimot'os and most low thyroid patients have it. Then it is a matter of calming down the autoimmune response. This is very possible and can make a huge difference in your life. Once that happens your energy, joy, and focus returns. And of course weight loss happens. Life is changed. Contact our office for more information.
Want to get fat? Go on a diet!
May 5th, 2016

It’s an addiction to insanity in our culture, one of the most overfed populations in human history — the weight loss diet.
Despite plenty of scientific evidence that diets don’t produce lasting results for most people and despite countless numbers of dieters, most of them women, thrown into a lifetime of damaging despair, low self-esteem, and self-hatred thanks to failing diets, our culture still blindly adheres to the low-calorie diet as the panacea for all life’s problems, including those extra pounds.
The reality TV show The Biggest Loser provided the perfect high-profile platform for scientists to showcase what millions of Americans have learned the hard way: diets make you fatter in the long run.
Why dieting makes you fat
For most of our species’ history, meager food supply and bouts of famine have been the norm. As a result, the body prioritizes conserving fat and energy through altering its metabolism and fat-storing hormones.
Metabolism slows dramatically for years
Eating fewer calories to lose weight significantly slows your metabolism and causes you to regain the weight quickly and easily. The body will fight for years to get back to its previous set point. Contestants on the Biggest Loser learned they now burn between 400 and 800 fewer calories six years after their televised weight loss journey. In other words, they have to under eat just to not continually gain fat.
Satiety hormones skewed for years
Diets also skew levels of leptin and other satiety hormones. These hormones control hunger and food cravings. All of the show’s contestants had normal levels of leptin prior to losing weight. After losing weight their leptin levels plummeted to near nil. A follow-up study showed after they had regained the weight leptin levels were at about half of original levels. Other satiety hormones were also out of range. This caused contestants increased hunger and cravings.
Televised torture for weight loss
The weight loss program The Biggest Loser contestants were put on not only ultimately damaged their metabolisms, it was unrealistic, tortuous, and exhausting. Contestants ate too few calories and exercised many hours a day, needing to quit their jobs to meet the weight loss demands. Maintaining the weight loss required exercising two to three hours a day and continued under eating. They were also left with mounds of loose skin.
Understand how the body works to lose weight
Fortunately, sustainable weight loss is possible for many people who understand functional medicine approaches to metabolism, satiety hormones, and the effects of stress and inflammation on weight. Unfortunately, those who have lost and gained weight repeatedly during their lives will have a bigger battle. It is also important to manage underlying causes of weight gain, such as emotional and addiction issues, PTSD, and chronic stress. For instance, one study showed many overweight women have been sexually abused as children.
Although portion control and regular physical activity are important, so too are managing the types of foods you eat. For instance, processed carbohydrates and sweets trigger the mechanisms that cause cravings and weight gain. On the other hand, consuming ample vegetables can alter the composition of gut bacteria in a way that fosters weight loss. Eliminating foods that are inflammatory, such as gluten in the case of gluten-sensitive people, can reduce stress on the body, thus facilitating fat burning.
And lastly, ditching the self-loathing and shame that accompanies diets can also reduce fat-promoting stress.
Ask my office for ideas on how to release weight in a way that is sustainable and healthy for the body. Call us at (952) 300-2260.
2016-02-08
Eat Breakfast if You Want to Lose Weight

If you’re like most Americans, you eat a high-carb breakfast packed with grains, dairy, and sugar, or you don’t eat breakfast at all either because you’re too busy or you want to lose weight.
Either way, you’re not doing yourself any favors.
Breakfast is exactly what it sounds like — the breaking of a fast. After 8-plus hours of no food, your body needs fuel to bring its systems up to speed and maintain even energy for the day. As it turns out, eating a solid breakfast is one of the best things you can do to lose weight. It also helps assure a clear mind, steady emotions, and plentiful energy throughout the day.
Skipping breakfast can actually make you gain weight!
We’ve all been taught the “calories in vs. calories out” theory for weight loss. In an effort to cut calories, we skip breakfast because it’s the easiest meal to do without, especially if we tend to wake up with no appetite or we’re always in a rush to get to work. But while calories can matter, skipping breakfast can actually lead to weight gain:
When you wake in the morning, your blood sugar is already low.
Skipping breakfast (or any meal) allows it to go lower and impairs insulin sensitivity, which leads to weight gain.
Chronic low blood sugar creates a cascade effect in your hormonal system that directly affects your body’s ability to deal with stress.
This can result in increased inflammation throughout your body, which can lead to weight gain. Low blood sugar also causes brain fog, mood issues, insomnia, decreased brain function, and other health issues. None of these symptoms will help you stick to a healthier eating plan.
Skipping breakfast has interesting behavioral effects; research shows that people who skip breakfast tend to reach for higher calorie foods once they do eat, leading to higher total daily calorie consumption than those who ate a solid breakfast. This is partly because missing meals causes the brain to become primed toward higher-calorie foods like it would during starvation or famine.
Skipping breakfast makes you more likely to binge on sugary foods that result in an energy crash later in the day—making you less likely to go out and get that much-needed exercise. (PS: A big sweet, milky coffee drink with whipped cream is not a breakfast.)
Eat a protein-strong breakfast for weight loss and steady energy
You know you need to eat breakfast. But eating traditional carb-heavy breakfast foods such as cereals, bagels, muffins, and fruit smoothies isn’t a great idea; they sabotage your weight loss goals by destabilizing blood glucose and insulin after the night’s fast, as well as kicking cravings for quick-energy sugary stuff and junk foods into high gear.
Eating a nutrient-dense, lower carb breakfast with plenty of protein and healthy fats provides the brain and body with proper fuel, balances your blood sugar and insulin, and gives your metabolism a boost for the day.
Studies show a protein-strong breakfast can also reduce hunger hormones, increase the chemical that tells your brain to stop eating, improve your sense of satiety, and reduce evening snacking.
2016-02-01
Loneliness is Bad for Your Health!
Everyone feels lonely from time to time. Maybe you miss a party, move to a new city, or lack a close circle of friends. Ideally, loneliness is temporary, but when it becomes chronic, it can have far-reaching consequences for our health. While we’ve known for decades that perceived social isolation, or loneliness, is a major risk factor for chronic illness and death, only more recently have we gained deeper clues into why loneliness is such a health risk.
Studies show loneliness affects immunity
In a study of overweight but otherwise healthy people, those with loneliness showed higher levels of inflammation when faced with stressful activities; another set of subjects experienced more inflammation, pain, depression and fatigue than normal, plus a reactivation of dormant viruses in the body. More recently, it was shown that loneliness reduced the ability to fight off viruses and bacteria.
Researchers say the body perceives loneliness as a stressor, causing it to go into a “fight or flight” response and release adrenal hormones. Over time this chronic stress response leads to chronic inflammation, setting the stage for numerous disorders, including depression, coronary heart disease, Type 2 diabetes, arthritis, Alzheimer’s disease, and cancer.
This explains why lonely people have been shown to be at increased risk for cancer, neurodegenerative disease, and viral infections.
Compounding the problem is the fact that chronic inflammation is linked with depression and other mental health issues, which may cause a lonely person to further isolate themselves in a vicious cycle that’s hard to break.
The remedy for loneliness
Clearly, healthy social relationships are the best antidote to loneliness. Relationships don’t just happen — you have to make them happen.
Ideas to remedy loneliness include: Join Meetup.com groups, or start one; schedule time with friends or acquaintances; attend local events; sign up for classes to learn something new with other people; join a volunteer organization; join a church or spiritual community. If you look outside yourself you will find a cornucopia of healthy social opportunities.
Humans are designed to commune. It’s vital to health because in our history it was vital to survival. The stress response to loneliness and isolation is a red flag that you need the feeling of protection and inclusion socialization brings.
If you feel depression and lack of motivation are holding you back from reaching out to form a healthy social community, ask my office about ways diet and specific supplementation can help boost your desire to socialize. Contact my office for more information: (952) 300-2260.
January 6th, 2016
Is PTSD Causing Your Chronic Stress or Fatigue?
Are you chronically stressed out, chronically fatigued, or both? Are you careful about your diet and lifestyle but nothing works? You may want to consider whether post-traumatic stress disorder (PTSD) plays a role in your poor stress-handling ability.
Studies show PTSD alters the body’s ability to regulate cortisol, our primary stress hormone produced by the adrenal glands. People with poor adrenal function suffer from usually either low cortisol or high cortisol.
Altered cortisol levels increase the risk for developing chronic conditions, such as autoimmune disease, chronic pain, or chronic inflammation.
More women suffer from PTSD than men
Not just war veterans suffer from PTSD. In fact, more women than men suffer from PTSD.
Why? For one, more girls than boys suffer sexual abuse as children, predisposing women to more severe reactions to traumas later in life. Researchers also found that sexual trauma causes more emotional suffering and is more likely to contribute to a PTSD than other types of trauma.
Women are also biologically more prone to PTSD than men.
Are your stress hormones to high or too low?
Low cortisol causes low blood sugar, blacking out when standing up, weakness and fatigue, waking up at 3 or 4 a.m., depression, hypersensitivity, and an inability to cope with stress.
High cortisol causes symptoms of insomnia, not feeling rested after sleep, weight gain around the abdomen, anxiety, chronic stress, and hormonal imbalances.
Supporting adrenal function is fundamental to good health. The first place to start is with diet, as many cases of low or high cortisol are simply a matter of too much sugar and too many processed carbohydrates.
Undiagnosed immune reactions to foods, such as gluten, dairy, egg, and soy can trigger adrenal issues.
An undiagnosed and chronic parasitic, viral, or bacterial infection can take their toll on the body’s stress handling abilities and cause low or high cortisol.
And, of course, lifestyle factors affect adrenal function. Over exercising, over working, not getting enough sleep, or being in a stressful job or relationship can certainly tax your adrenals and lead to altered cortisol.
But if you have been addressed all those and low or high cortisol persists, it’s time to investigate whether PTSD is a contributing factor.
Past traumas and even your parents’ traumas can cause poor adrenal function
Studies have shown that PTSD can cause low or high cortisol. An interesting finding is that people tend to have low cortisol if both parents suffer from PTSD. This is likely due to both the biological effects of PTSD as well as the child’s environment growing up.
Research has also found that low cortisol is more often associated with the PTSD symptoms of avoidance, withdrawal, and isolation, while high cortisol is associated with hyper arousal and re-experiencing traumatic events.
Cortisol plays a significant role in your physical and mental well-being and if you suspect you may have PTSD, it’s important to seek non-pharmaceutical treatments. Fortunately, PTSD is much studied these days and many treatment options exist. Contact my office for more information about PTSD and chronic stress and fatigue.
December 31, 2015
Recovering from Sugar and Alcohol Hangovers
With the promise of good intentions around the corner, the end of the year can turn into a downward spiral of too much sugar and alcohol.
It’s hard to get back on the healthy eating wagon, but knowing a few things about how sugar and alcohol affect the body can help.
Recovering from the sugar hangover
Has a sugar hangover left you with an upset stomach, a headache, brain fog, skin issues, chronic pain, mood swings, allergy symptoms, lethargy, and self-loathing?
Steps for recovering from a sugar hangover include:
1) No sugar. Holiday desserts shoot your blood sugar levels up and down. This taxes the immune system, imbalances brain chemistry, and skews hormones. To stabilize blood sugar, eat protein every two to three hours, never skip breakfast, and avoid sweets and starchy foods. Focus on proteins, vegetables, and healthy fats
2) Hydrate. Staying hydrated with filtered water will help flush toxins from your body.
3) Support your liver. Help your liver flush toxins with compounds such as as milk thistle, dandelion, N-acetyl L-cysteine, beet root, panax ginseng, and more.
4) Heal your gut. Unstable blood sugar inflames the gut and promotes yeast and bacterial overgrowth. In addition to stabilizing blood sugar, follow the autoimmune paleo diet that eliminates common immune triggers (such as gluten), and use gut support compounds like probiotics and L-glutamine.
5) Exercise. If you’ve been morphing into the couch, go easy initially to avoid more inflammation. Appropriate exercise will help tame inflammation, improve brain function, and help flush toxins.
Recovering from the alcohol hangover
Alcohol hangovers are their own special hell.
We don’t fully know why hangovers happen, but a few facts can help us recover from them.
Alcohol blocks the production of a hormone that helps the body absorb water. As a result, the body immediately excretes the water—up to four times as much as the alcohol consumed. This is what causes fatigue, dry mouth, and a headache. Drink plenty and use electrolytes to help rehydrate.
When that water is excreted, many of our water-soluble vitamins go with it, contributing to that lousy hung-over. A b-complex supplement before drinking and another the next day can help compensate.
Alcohol also breaks down the body’s store of glycogen, an energy source, thus causing weakness, fatigue, and lack of coordination. It’s important to remember to eat.
Drinking alcohol creates the powerful toxin acetaldehyde in the body. The body attacks it with an antioxidant called glutathione, our body’s most powerful antioxidant. Using natural compounds to support glutathione can help with recovery.
Alcohol inhibits glutamine, one of the body’s natural stimulants. When you stop drinking, the body responds by producing more than it needs, disrupting sleep and causing hangover tremors, anxiety, restlessness, and increased blood pressure. Allow yourself to take it easy.
The New Year is a great time not to focus on unrealistic goals, rather on simple daily strategies to not only recover from holiday excesses but also improve how you feel and function all year. Ask my office for more advice.
November 11, 2015
WHY YOUR NEGATIVE GLUTEN TEST MAY HAVE BEEN WRONG
If you tested for whether gluten might be behind your chronic health issues but a blood test came back negative, are you wondering, “Now what?”
Although it’s possible gluten may not be a problem for you, there’s a high probability that test result was inaccurate. Conventional testing for gluten sensitivity misses many important markers and can give you a false negative result. As a result, you may be told gluten is not an issue when in fact it is provoking your autoimmune disease or chronic health condition. Gluten has been linked in the literature to 55 diseases so far, most of them autoimmune.
Fortunately, newer testing has been developed by Cyrex Labs to catch the cases of gluten sensitivity that conventional testing misses.
WHY STANDARD BLOOD TESTS OFTEN FAIL AT DIAGNOSING GLUTEN SENSITIVITY
Standard blood tests for gluten sensitivity have a less than 30 percent accuracy rate. Gluten has to have significantly destroyed the gut wall for blood testing to be effective. In many people, gluten damages other tissues in the body, such as neurological tissue.
Current tests only screen for one component of wheat, alpha gliadin. Yet people can react to at least 12 different portions of the wheat protein.
In some people, other foods such as dairy can trigger a gluten-like immune response because the body sees them as one in the same. This is called cross-reactivity. Conventional doctor’s offices do not screen for this.
Standard testing only looks at the response of one set of immune cells. If those cells are depressed due to immune exhaustion, results could be inaccurate. More thorough testing compensates for immune depression by testing a variety of immune cells.
GLUTEN DAMAGES MORE THAN THE GUT
Standard testing also only looks at whether gluten sensitivity is destroying gut tissue. However, in many people, gluten does not cause an immune reaction in the digestive tract to the same degree it does in the brain or in the skin. In fact, most people are affected neurologically by a gluten intolerance. Fortunately, we now have ways to screen for that.
WHICH PART OF WHEAT DO YOU REACT TO?
Gluten sensitivity isn’t as cut-and-dry as once thought. (Also, the word “gluten” is technically incorrect as “gliadin” is the portion of wheat that triggers an immune response.)
Wheat is made up of more than 100 different components that can cause a reaction, not just the alpha gliadin component most tests use.
Other parts of wheat that can cause gluten sensitivity include different forms of gliadin besides alpha gliadin, the portion of wheat found in whole wheat, the sticky portion of gluten, wheat that has been altered through industrial processing, and wheat opioids — substances produced during the digestion of wheat that have additive properties similar to opiates. People with a wheat opioid sensitivity may go through severe withdrawals on a gluten-free diet.
ADVANCED GLUTEN SENSITIVITY AND IMMUNE TESTING
In addition to comprehensive gluten sensitivity testing, Cyrex also tests for the following: foods that cross react with gluten, damage that gluten can cause to your gut and your brain, and autoimmune reactions (when your immune system attacks and destroys body tissue) that may have gone undiagnosed yet cause chronic symptoms. For more information about advanced immune testing, contact my office: (952) 300-2260
November 9, 2015
It seems almost everyone has insomnia these days, including, possibly, you. People either can’t fall asleep, they wake up after a few hours of sleep and can’t go back asleep, or they aren’t able to sleep deeply. The reasons for

insomnia vary from person to person, but it’s typically not due to a sleeping pill deficiency.
In this article I’ll go over often overlooked issues that cause insomnia and poor sleep. Don’t assume a powerful sleeping pill is your only answer. Look at the underlying causes first and address those.
5 THINGS THAT CAUSE INSOMNIA
1) Low blood sugar. Do you wake up at 3 or 4 a.m., racked with anxiety and unable to fall back asleep? That could be caused by a blood sugar crash, which raises stress hormones (hence the anxious wake up). Eating small but frequent meals, never skipping meals, and avoid sugary and starchy foods are important to keep blood sugar stable. Additionally, eating a little bit of protein before bed and at night if you wake up may help.
2) High blood sugar (insulin resistance or pre-diabetes). Do you fall asleep after meals yet struggle to fall asleep at night? Do you wake up feeling like you’ve been run over by a truck, but are wide awake at bedtime? It could be high blood sugar, a precursor to diabetes, is driving your primary stress hormone cortisol and keeping you up. A telltale symptom of high blood sugar is falling asleep after meals, especially starchy meals. Minimizing sugary and starchy foods, not overeating, and exercising regularly can help you rewind insulin resistance and sleep better at night.
3) Too much blue light. Are you staring into a computer, phone, tablet, or TV screen right before bed? If so, you’re confusing your body’s sleep hormone production. The body recognizes blue light as daylight, which suppresses the production of melatonin, our primary sleep hormone. Limiting your exposure to blue light at night can help boost your body’s production of sleep hormones. Wear orange glasses two hours before bed, use orange bulbs in your nighttime lamps, and limit your evening screen time to boost melatonin.
4) Inflammation. If you are chronically inflamed it drives up your stress hormones, which can keep you awake. This is particularly true if you’re experiencing inflammation in your brain, which can cause anxiety. One of the most common causes of chronic inflammation is an immune reaction to foods, especially gluten, dairy, eggs, and various grains. Screening for undiagnosed food sensitivities and an anti-inflammatory diet can help you hone in on what’s causing your insomnia or poor sleep.
5) Hormone imbalances. Hormone imbalances can significantly impact sleep. Low progesterone, which is a common symptom of chronic stress, heightens anxiety and sleeplessness. An estrogen deficiency in perimenopause and menopause has been shown to increase anxiety, insomnia, and sleep apnea. In men, low testosterone is linked with poor sleep and sleep apnea. Also, low hormone levels can be inflammatory to the brain, increasing anxiety and insomnia.
Many things can cause insomnia and poor sleep, however these are some of the more common. While you are addressing the underlying factors of your sleep issue, you can aid your ability to sleep with safe and natural compounds, depending on the mechanism.
October 29, 2015
GOT BRAIN DRAIN? GO GRAB YOUR PEN AND PAPER!
Do your fingers whir across the keyboard, leaving your brain in the dust? The remedy could be as simple as putting a pen to paper for a little bit each day. Research shows that although keyboards make writing fast and easy, they also make for sloppier brain function compared to handwriting.
Handwriting has been phased out of everyday life and school curriculum. Studies show many people can’t remember the last time they had to write something by hand and many children don’t know how to properly hold a pen or pencil because it’s barely taught in school.
This is bad news for our brains, say experts. The reason it takes children several years to learn how to write is because writing requires so many different areas of the brain to work simultaneously, enhancing development.
Likewise, college students who take notes by hand understand the material better than computer note takers. Note taking by hand requires more focus and discernment, enhancing memory, while taking notes on a laptop note can turn into mindless transcription.
In fact, taking notes by computer actually impairs the learning process while handwriting enhances it, thanks to the motor skills involved.
WHY HANDWRITING IS BETTER FOR THE BRAIN
Neuroscience has discovered a variety of reasons why handwriting is better for the brain than typing.
• It activates brain pathways involved in learning.
• It stimulates more ideas and creativity.
• Cursive writing can help remedy dyslexia.
• Taking notes by hand improves memory.
• A handwritten piece has more personality than something type written, thus improving human connection.
Handwriting involves fine motor skills that involve more areas of the brain in the learning process.
Perhaps those missing out most on the neurological benefits of handwriting are the children who barely learn it. Cursive writing is largely no longer being taught and keyboard proficiency takes precedence over writing after first grade.
Brain scans of children learning letters through writing versus through typing showed writing activates various parts of the brain while typing hardly activates it at all. In other words, those messy first stabs at writing that gradually improve with practice are building neurological foundations that make learning easier and more enduring.
IMPROVE YOUR HEALTH WITH HANDWRITING
Because it boosts brain function, handwriting can improve your health. You can further supercharge the benefits of handwriting based on what you write about. Look what studies show:
• Writing down your thoughts and feelings can make your wounds heal faster.
• Writing 20 minutes a day improves quality of life for patients with cancer.
• People who keep a gratitude journal are more optimistic and exercise more.
• Writing down what you’re grateful for at night can improve sleep.
• Expressive writing has been shown to improve mental and physical well-being.
Whether you keep a gratitude journal, take class notes by hand, or commit to regularly writing an older relative handwritten letters (which will be deeply appreciated), handwriting is a small but effective way to boost your quality of life.
Talk to our office for more details on how you can improve your brain health- Or send us a handwritten note TODAY! 8120 Penn Ave S, #120 Bloomington, MN 55431
October 22, 2015
Why High Blood Sugar Can Cause Deadly Diseases
It’s not easy being a healthy American. We are constantly besieged by the lure of sugary, starchy treats (salted caramel latte and a scone anyone?). Yet behind the innocent disguise 
Heart disease, stroke, diabetes, arthritis, and Alzheimer’s are among the most common and expensive health problems in the United States. In most cases their origins spiral back around to those small daily decisions — the fries instead of a salad, the syrupy hot drink with whipped cream instead of a simple cup of coffee or tea, or the ice cream or pie for dessert instead of a little fruit (or -- GASP! -- no dessert).
What is it about these seemingly innocuous indulgences that add up to deadly diseases? Sugar and refined carbohydrates.
(Although the hydrogenated fats, lack of fiber, industrialized salt, and artificial chemicals play their roles, too.)
The standard American diet chronically spikes blood sugar, which in turn chronically spikes inflammation. Inflammation is now recognized as the common denominator among chronic disease today.
Stable blood sugar levels are vital to all processes of the body, especially those of the brain and the immune system. The body has a variety of mechanisms in place to keep blood sugar within a narrow range. Americans, however, exhaust this system with a degree of sugar consumption our bodies were not designed to handle.
Pasta, white rice, breads, pastries, soda, coffee drinks, ice cream, etc. — are examples of foods that spike blood sugar.
How sugar and insulin lead to chronic disease
Too many sugars and processed carbs cause the body to overproduce insulin, a hormone that escorts glucose into cells and helps regulate high blood.
This constant over production of insulin exhausts the body’s cells. In an attempt at self-defense, they refuse entry to the insulin. This is called insulin resistance.
Now glucose is unable to enter into the cells where it’s needed to make energy. This explains why people feel sleepy after eating, especially after eating sugar, high-carb meals or overeating.
Another reason is because excess sugar must be taken out of the bloodstream, so the body converts it to fat. This is an energy-demanding process that also contributes to post-meal sleepiness.
This excess sugar in the bloodstream is highly damaging, damaging blood vessels and the brain, and triggering an inflammatory response.
Research shows links between insulin resistance and many chronic diseases, including heart disease, stroke, cancer, diabetes, arthritis, and Alzheimer’s. Some researchers call Alzheimer’s type 3 diabetes because sugars damage the brain.
To make things worse, because of the damaging effects of insulin resistance and high levels of circulating glucose, people with insulin resistance often feel too tired to exercise, are prone to overeating, and have intense sugar cravings.
Symptoms that indicate risk of chronic disease
Symptoms of insulin resistance that can raise your risk of chronic disease include:
• Fatigue after meals
• General fatigue
• Constant hunger
• Constant craving for sweets
• Strong desire for sweets after meals
• Waist girth equal to or larger than hip girth
• Frequent urination
• Increased appetite and thirst
• Difficulty losing weight
• Migrating aches and pains
One of the best ways to prevent or manage chronic disease is to eat a diet that stabilizes your blood sugar. Regular exercise also increases insulin sensitivity. Certain nutritional and botanical supplements can help manage insulin resistance. Contact my office for to set up a consultation today: 952-300-2260
October 15, 2015
How to Overcome: YOUR ADDICTION TO UNHAPPINESS
Notice how easy it is to hang on to anger, shame, guilt, worry, and other negative emotions? Are these emotions so horribly delectable you just can’t let go?

You’re not alone. However, you could be worsening your health by giving in. Scientists have discovered negative emotions have an addictive quality that trigger the reward centers in the brain. In other words, you feel like you’re rewarding yourself when you succumb to negative emotions.
Worry activates areas of the brain that trick you into feeling soothed. Pride and its shadow twins of shame and guilt are the most powerful triggers of the brain’s reward centers. On some twisted level, these yucky emotions feel good.
As with many addictions, negative emotions are fine in moderation (and even beneficial), but toxic when indulged in regularly. They raise stress and inflammation, our two biggest foes when battling autoimmune disease and chronic illness.
Four scientific tips to boost happiness:
Happiness is effortless for some people. Good for them. The rest of us have to work at positivity the same way we do at diet and exercise.
If you’re a pro at managing your autoimmune disease through diet and lifestyle, don’t overlook how influential feelings and attitude are on your health.
Here are some tips from a neuroscientist to wean yourself off an unhappiness addiction:
1. Activate the reward center of the brain with gratitude instead of negativity. Shame, guilt, and worry trigger the same brain chemicals gratitude does. Except gratitude doesn't make you sick; it improves health.
Don’t have anything to be grateful for (c’mon…)? Doesn’t matter. It’s the searching for gratitude that elicits positive benefits.
2. Label negative feelings. Labeling your negative feeling in a few words activates different areas of the brain that lighten the negativity load. Practicing mindfulness is healthier than suppressing emotions.
3. Make a decision when overcome with worry and anxiety. When you’re besieged by worry, create an intention, set a goal, take action — just do something. This boosts the reward center of the brain and takes it off that exhausting hamster wheel. Don’t trap yourself with making the best decision or the one you should make. Instead, shoot for a “good enough” decision that you make for you.
4. Socialize and touch. Appropriately, of course. As far as the brain is concerned, social exclusion is an injury while healthy socialization is an elixir. Even little touches — handshakes, pat on the back, tap on the arm, a hug — amplify the health benefits of socialization. Got no one to touch? Get a massage. And don’t rely solely on texting or the Internet for your socialization. Research shows they don’t impart the same benefits “in-real-life” human company does.
Basically, working towards positivity exercises your brain and helps pull it out of destructive, self-perpetuating loops that raise stress hormones and drive inflammation. Brain exercises aren’t just about crossword puzzles and Sudoku — you also need to exercse the brain’s positivity centers. Ask my office for more information on brain health.
Think you don’t need your gallbladder? Think again.
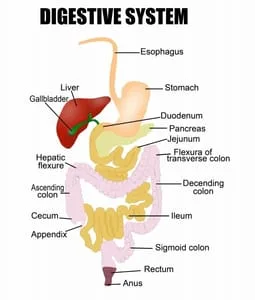
Have you been told you don’t need your gallbladder? Think again. Sure, you’ll live without it, but the gallbladder is actually a vital digestive organ.
The gallbladder stores bile, a chemical made by the liver that emulsifies fat, and secretes it into the small intestine when needed.
Bile is necessary for the digestion and absorption of fats, and it helps ensure you absorb vitamins and minerals from foods in your diet.
Gallstones and a congested gallbladder
Gallbladder removal is one of the most common surgeries today and is performed when the gallbladder becomes congested with gallstones.
Things that can cause gallstones are nutritional deficiencies, hydrogenated fats (trans fats), processed vegetable oils, hypothyroidism, and no-fat or low-fat diets.
The gallbladder there is like a holding tank for bile that secretes it as needed, such as when you eat something fatty.
Without a gallbladder the liver continuously leaks bile into the small intestine.
This means there is not enough stored bile to digest fats. As a result, fats can be become rancid and irritate and inflame the digestive tract. This can result in not only discomfort, but also poor digestive function and inadequate absorption of nutrients.
If you have a gallbladder but it’s sluggish and congested with stones, this backs up the liver’s detoxification pathways. As a result, the liver cannot effectively detoxify hormones, toxins, and other metabolites.
Things to watch out for if you’re gallbladder has been removed
Gallbladder removal puts you at risk for deficiencies of essential fatty acids, which are vital for good brain health and hormone function, and fat-soluble vitamins, such as vitamin D, A, and E, which are especially important for good immune health.
Also, if the gallbladder isn’t there to emulsify fats, the health of the entire digestive tract may become compromised. Studies suggest gallbladder removal increases the risk of colon cancer.
How to support gallbladder health
Luckily, various nutritional compounds support gallbladder health, fat digestion, and liver detoxification, including dandelion root, milk thistle seed extract, ginger root, phosphatidylcholine, and taurine.
These compounds can also help if your gallbladder has been removed, along with ox bile.
Maintaining good gallbladder health
- Following are some tips to support good gallbladder health:
- Eat a diet high in fiber
- Avoid trans fats, hydrogenated fats, and processed vegetable oils
- Get plenty of essential fatty acids and omega 3s
- Eliminate food intolerances
- Make sure to properly support low thyroid function or autoimmune Hashimoto’s hypothyroidism
Ask my office for more advice on how to support your gallbladder or your digestive health if your gallbladder has been removed.
SEPTEMBER 28, 2015
Is your brain inflamed? How to tell and what to do
When most people think of inflammation they think of arthritic joints, or maybe a sprained ankle. But did you know your brain can become inflamed, too?
The problem is an inflamed brain won’t hurt. Instead you should look for other symptoms of brain inflammation. These include brain fog, slow thinking, fatigue, and depression.
Brain fog is a hallmark symptom of brain inflammation. The inflammation slows down communication between neurons. This is what causes you to feel foggy, dull, and slow.
Brain inflammation is serious because it means nerve cells in the brain are dying. In other words, brain inflammation is causing your brain to atrophy and age too fast.
What causes brain inflammation
A common cause of brain inflammation is head injury. Injuries cause immune cells to turn on in order to begin the healing process. But unlike immune cells in the body, the brain’s immune cells do not turn off. This means brain inflammation can continue to be a problem long after the injury. This is one reason football players have high rates of the chronic degenerative brain disease called chronic traumatic encephalopathy.
Other common causes of brain inflammation include chronic inflammation in the body, leaky gut, high blood sugar and diabetes, hormone imbalances, hypothyroidism, food intolerances (gluten is a notorious brain inflamer), stress, and brain autoimmunity — a disorder in which the immune system erroneously attacks and damages brain tissue. It is more common than people realize.
Depression and brain inflammation
Depression is a common symptom of brain inflammation (although different things can cause depression, depending on the person). Immune cells called cytokines that are created by inflammation impair brain function. Cytokines also hamper the activity of serotonin, the “joy and well-being” brain chemical commonly linked with depression.
A good illustration of this is the fact that many patients given the anti-viral drug interferon, which increases cytokine activity, develop depression. Conversely, many people who address inflammation relieve depression.
Brain inflammation: Autism to Alzheimer’s
Brain imaging and autopsies show brain inflammation is more common in individuals with autism.
Brain inflammation is also increasingly being linked with dementia and Alzheimer’s disease. The inflammation both degenerates brain tissue and increases amyloid beta, the hallmark of Alzheimer’s.
Take brain inflammation seriously to save your brain
If you have brain fog or other symptoms that suggest brain inflammation, this means your brain is degenerating (aging) too fast. Be proactive in saving your brain health:
- ·
- · Low blood sugar, insulin resistance (high blood sugar), and diabetes
- ·
- · Low sex hormones (such as estrogen
- · inflamed gut causes an inflamed brain.
Take glutathione precursors. Glutathione is the body’s master antioxidant and can help quench brain inflammation. Sufficient essential fatty acids and vitamin D are important, too.
Lack of sleep: Early mornings cause gene changes
We all want enough sleep so we’re less cranky and more alert. We want it for our kids too. But recent research found an even more important reason: Sleeping less than six hours a night for one week can lead to more than 700 changes in the way our genes behave. Among these are genes that regulate stress, our ability to fight disease, our sleep-wake cycles, inflammation, and aging.
Researchers believe this helps explain why chronic sleep deprivation is linked to heart disease, diabetes, obesity, stress, and depression.
Sleeping less than five hours a night has also been linked with greater risk of death.
Early mornings hard on youth
Researchers are increasingly sounding the alarm about the ill health effects of early mornings. They suggest elementary school start at 8:30, middle and high school at 10 a.m., and university classes at 11 a.m.
These wake up times better match the body’s natural circadian rhythm, or sleep-wake cycle. Early starts are particularly onerous on youth because sleep is when they develop mentally, physically, and emotionally. Sleep deprivation can also be fatal as sleep-deprived teens are more likely to get in car accidents.
One study found British students were losing an average of 10 hours of sleep a week, making them more deprived than doctors on a 24-hour shift.
Another study of 900,000 children globally found American youth are the most sleep-deprived.
Most workers should start the day at 10 a.m.
Children and teens aren’t the only ones who should start the morning later. Research has also found early work times are not in sync with the internal clocks of working adults in their 20s and 30s. In fact, the nine-to-five day is best suited only for children under 10 and adults over 55.
Meanwhile, young people between the ages of 14 and 24 are the most sleep-deprived group of any age sector. This translates to a more drastic impact on gene expression that can raise the risk of various health disorders.
Limit screen time at night to facilitate sleep
Although our body clocks may be more in tune with later wake times, poor habits play a role in sleep deprivation, too.
Adults and children are on their smart phones and tablets late into the night, not only forcing themselves to stay up too late, but also over-exposing their internal clocks to too much “artificial daylight.”
The blue light emitted from LED screens used on smart phones, tablets, computers, and LED televisions are similar to the daylight.
This suppresses the release of melatonin, the sleep hormone, while keeping the adrenal hormone cortisol active. The result is insomnia and poor sleep.
It’s important to limit screen time at night. If that seems like too much to ask, wearing orange tinted glasses can limit the blue wavelengths from entering the eyes and induce evening sleepiness.
A small study of Swiss teen boys showed they felt significantly more sleepy at night after wearing the glasses at night for just one week. Also, apps for your devices such as f.lux reduce blue wavelengths emitted from your screen as the sun goes down, resulting in less eyestrain and better sleep at night.
Poor sleep can have many causes including those I've already mentioned, but also blood sugar imbalances, hormonal imbalances, brain-based issues, and more.
Ask my office for more advice on improving your sleep via email at [email protected] or via phone at 952-300-2260

August 19, 2015
Eat better and be healthier with batch cooking

Does a demanding schedule prevent you from cooking healthy? Busy lifestyles can send our eating habits down the drain, with our health and nutrition following right behind it. Many common health issues can arise as a result.
The solution? Batch cooking! Batch cooking is an organized system to plan, create, and utilize meals, saving you an incredible amount of time, energy and effort.
In two sessions a week, you can prepare an entire week’s worth of meals. People report reducing 20 to 30 hours of cooking and cleanup per week down to four or five! This set of simple guidelines will help you get started:
Planning your menu
- Pick simple, nutrient-dense recipes and save unfamiliar, complicated ones for their own special time.
- Try to choose one-pot/skillet/casserole recipes, with a minimum of side dishes.
- If you’re making a meal that uses protein such as a roast or chicken, make extra to use in simple meals later in the week, such as salads or soups.
- Plan for every meal of the week, not just dinners.
- Make a written menu (and grocery list) so that when you pull a meal from the freezer on Tuesday night, you know which side dish goes with it on Wednesday. Also, write down timing for when a meal needs to be pulled from the freezer.
- Write down all the parts that need preparing so you stay organized.
- If making all oven dishes, make sure they use the same oven temperature so you can do them all at once and save time.
- Another option: Choose a variety of meals that use either stove top or oven, so you don’t over crowd either location.
Kitchen logistics
Know what kitchen tools you’ll need and don’t double up on recipes that need them. For example, if you need the food processor for three dishes in one session, it will take more time.
Do you have the amount and type of storage containers that you’ll need?
Plan your dishes with fridge/freezer space in mind. Look at which dishes can be frozen for later and which must go in the fridge and be consumed within two days.
Putting your apron on
- Choose one to two days a week for batch cooking, and dedicate two to three hours for each session. It may take you less time once you develop your own rhythm and familiar recipes.
- If you have young children who demand a lot of attention, try to plan it for while they are out of the house.
- Start with a clean kitchen; you’ll have what you need at your fingertips, and it’s easier to keep a clear head.
- To save time, do all the prep work at the beginning, not between dishes.
- Use a timer; you’re multi-tasking and could forget something.
- Clean as you go to save time.
- Package the food in serving-size portions that are easy to defrost or serve from the fridge.
- Always label each meal with masking tape and a Sharpie marker. You might not recognize a dish once it’s covered in frost!
- Make sure you’re well fed and hydrated before and during your batch-cook session to help keep your brain sharp and your energy level stable.
Special tips
Always have a couple extra meals stashed away in the freezer as last-ditch emergency meals to use only when you truly need them – such as when you get back from vacation.
For people who feel overwhelmed in general, batch cooking can seem daunting. However, everyone who batch cooks develops their own rhythm and system with practice, and this set of simple guidelines will help you get started. Remember, the time you dedicate to planning your menu and making the food for each week will be more than paid off in saving time and energy when you hit the fridge or freezer to rustle up a meal. Most of the effort is in the planning; once you put on that apron, it’s easy to just keep rolling!
If you love the idea of batch cooking but want more information, check out this resource.
August 17, 2015
How to avoid those daily afternoon crashes

Even though it’s fairly common, the “afternoon crash” isn’t normal. Instead it’s a sign of unstable blood sugar, which wreaks havoc on the rest of your body’s systems. The afternoon crash means your blood sugar has dropped too low for your brain and body to function normally, causing you to become drowsy, mentally foggy, tired, and unmotivated.
The first thing most people reach for is a quick fix — caffeine or sugar. These may wake you up for a while, but they send an already imbalanced blood sugar system into another roller coaster ride of peaks and plunges. When this happens on a regular basis (several times a day for most people), it sets you up for chronic blood sugar imbalances including hypoglycemia and insulin resistance, a precursor to adult-onset diabetes.
How to avoid the afternoon crash
Wondering how to survive until dinner without a croissant and tall double mocha?
1. High protein breakfast: Eat a high-protein breakfast with plenty of healthy fats such as olive, avocado or coconut oil; a minimum of carbohydrates; and no added sugars or sweeteners. This provides your body with the necessary nutrients to bring it up to speed after a night of fasting (thus the word “break fast”), and allows your blood sugar to stabilize and get on a steady plane for the day.
Two examples:
• Turkey sausage with steamed greens and sweet potatoes.
• Smoked salmon or two eggs with sliced avocado, sauteed vegetables, and half a baked yam.
The idea of a savory breakfast might sound strange if you’re used to cereal or toast, but your body will quickly thank you for it. You’ll also notice a difference at 3 p.m.!
2. Avoid fruit, high-carb foods, and added sugars: Every time you eat fruit, high-carb foods (such as white rice, bread or noodles), and added sugars, you spike your blood glucose and the body has to struggle to bring it back into balance. Do this too often or too dramatically, and you can damage your body’s ability to handle glucose properly, causing hypoglycemia and/or insulin resistance (yes, you can have both at the same time). Blood sugar imbalances also create a hard-to-fight cycle of craving and bingeing.
TIP: Always eat a bit of protein or fat when you have something sweet to slow down the uptake of glucose and a blood sugar spike.
3. Energy crash? Eat smart: If you find yourself slipping into the afternoon blahs, don’t reach for stimulants or sugar, no matter how much your brain shouts for them. Instead, grab a snack high in protein and healthy fats, with perhaps a bit of healthy carbs included. This powers your brain with useful nutrients and avoids the blood sugar crash that follows a caffeine or sugar binge. And don’t forget — if you have a mid-morning snack, the same rules apply. Two snack examples:
• A quarter cup of pecans and a handful of plantain chips.
• A boiled egg with sliced carrots and avocado.
TIP: prep your morning and afternoon snacks each night before bed, so you can bring them to work and avoid the panicked rush to the café or candy machine.
4. Caffeine in moderation: Caffeine is hard on your adrenal glands, the glands that manage how you deal with stress. If you would rather give up your right arm than your daily cuppa, just make sure you drink that coffee early in the day, and make it a single shot. Even better, learn to love a healthy, brain-energizing drink such as kombucha or a veggie smoothie. They make great conversation starters at the water cooler, too!
Follow these guidelines and you’ll find yourself easing out of those afternoon crashes. Your energy will be more consistent throughout the day and you won’t feel the need to resort to snacks that spike and crash your blood sugar, brain function, and energy level. Feeling doubtful? Try it for a week and then decide.
August 10, 2015
Seven reasons exercise recovery can be difficult

If recovering from exercise is so difficult it feels like it’s ruining your days and sapping your motivation, you may be suffering from loss of exercise tolerance. Exercise is supposed to make you feel better and give you more energy, not make you feel worse.
The occasional off day is nothing to worry about, but if you find you’re consistently having a hard time handling your workouts, it’s important to find out why.
Symptoms of poor exercise recovery
- Can’t complete normal workouts
- Difficulty recovering after exercise
- Need a nap after exercise
- Unexplained depression
- Loss of general motivation or enthusiasm
- Unexplained change in weight
- Aggression or irritability for minor reasons
- Weakened immune function
- Loss of menstrual cycle
- Symptoms of leaky gut
Seven things that can cause poor exercise recovery
1. You’re overtraining: It’s possible you’re simply taking too much on during your workout. Anyone can make this mistake. Try backing off for a couple weeks; if your symptoms change, this could be your answer.
2. Your body wants a different kind of workout: Ways to exercise include extended aerobics, high intensity interval training, and weight training. Try a different form of exercise for a few weeks and see how you feel.
3. Insufficient protein intake: The U.S. RDA for protein is .08g per kg of body weight per day (1lb=2.2kg). Macronutrient requirements vary depending on age, health, and diet, but for some this may be too little to recover. Many active people feel better eating protein at rate closer to 1.4 to 1.8g/kg daily. Do the math and experiment with your protein intake.
4. Inappropriate carbohydrate intake: How many carbohydrates one should eat is a controversial topic, but at the end of the day we’re all unique. If you frequently feel run down you may be eating too many carbs … or too few. Too many carbs can cause blood sugar to skyrocket and plummet so energy levels crash. Too few can short you on fuel so that energy lags. This is especially true if you have adrenal fatigue and are struggling to adapt to a low-carb diet. Experiment adjusting your carb intake with healthy produce-based carbs, such as sweet potatoes.
4. Not enough sleep: Sleep is key to exercise recovery. Are you getting the recommended seven to nine hours a night? If you’re having unexplained sleep problems, ask my office for advice as many health issues can cause poor sleep
5. Micronutrient deficiencies: Staying well nourished can be difficult if you’re busy. If your body is low in vital nutrients such as Vitamins D and B12, iron, and other minerals, it can affect your ability to recover from exercise. Ask my office about making sure you’re meeting your micronutrient needs.
6. Low adrenal function: Your adrenal glands are the walnut-sized glands atop each kidney that manage your body’s ability to deal with stress. Americans are stressed out and as a result many people suffer from compromised adrenal function. This is a common cause of constant exhaustion and an inability to recover from exercise. If you’ve lost your get-up-an-go, adrenal function is one of the first things to consider.
7. Chronic inflammation: If you have an autoimmune disease that is not being managed or that is constantly flaring, or if you suffer from chronic inflammation, this will hamper your ability to recover. Examples of autoimmune disease include Hashimoto’s hypothyroidism, type 1 diabetes, or psoriasis. Symptoms of chronic inflammation can include joint pain, digestive difficulties, inflamed skin, or brain fog. If your body is already struggling to function in the face of chronic inflammation, exercise will put it over the edge and recovery will be difficult.
These are some common factors that can hamper exercise recovery, although there are many more, such as compromised thyroid function or a defect in your MTHFR gene, which plays a role in detoxification and metabolism. Untreated MTHFR can affect energy levels. Fortunately, it’s easy to diagnose and treat.
Any time you notice a change in your energy level or ability to recover from exercise, there is a reason. Don’t push it, and don’t ignore it. Ask my office for support in helping you find underlying causes of poor exercise recovery so you can feel and function better.
August 3, 2015
Adrenals wrong target with stress and Hashimoto’s

When stress levels go too high when you have Hashimoto’s hypothyroidism, the first thing many in the alternative health do is support the adrenal glands. The adrenal glands are two walnut-sized glands that sit atop each kidney and secrete stress hormones. Popular supplements include adrenal glandulars (adrenal tissue from animals), minerals, B vitamins, and a variety of herbs — all focused on boosting the ailing adrenal glands.
Although this is a sometimes a valid approach, more often the real target for support should be the brain. The adrenal glands simply take orders from the brain to manufacture and secrete adrenal hormones such as cortisol, our primary adrenal hormone. The brain has stress pathways that sometimes need support.
When stress becomes chronic and intense, the adrenal glands flood the brain and body with too many stress hormones. This exhausts the adrenal glands and eventually they fail to make enough cortisol. When this happens you don’t have the energy to handle even mild stressors, such as a common virus or a bad day at the office. As a result, fatigue sets in and your overall quality of life diminishes. Fatigued adrenal function also makes it difficult to manage autoimmune conditions such as Hashimoto’s.
Although the adrenal glands may need support, the best thing to do is target your brain health for stress support. This will not only help you feel better but also slow down brain degeneration. Chronic stress has been shown to literally cause the brain to atrophy, or shrink. In turn, a degenerating brain stresses the body, creating a vicious cycle. Unmanaged Hashimoto’s hypothyroidism is also very hard on the brain, delivering a double whammy. That’s why with Hashimoto’s it’s always important to include brain health in your protocol.
One of the first things to look at when supporting brain health is whether it is getting enough of the basic nutrients it needs, such as essential fatty acids and methyl B-12. Are you low in vital brain chemicals, called neurotransmitters, such as serotonin or GABA? Are you sending enough oxygen to the brain with good circulation, which is best boosted by exercise? Do you have anemia or blood sugar imbalances that rob the brain of good health and function? All of these imbalances also make it more difficult to successfully manage Hashimoto’s hypothyroidism.
Nutritional compounds that support healthy stress responses and target the brain include phosphatidylserine, which dampens the effects of the inflammation caused by stress on the brain.
Herbs called adrenal adaptogens also have a powerful effect on stress pathways in the brain. They include Panax ginseng extract, ashwagandha, Holy basil extract, Rhodiola rosea, and eleuthero. They have a synergistic effect when used in combination — ask my office about adrenal adaptogens.
Too much stress inflames the brain, which compounds stress and ages the brain too quickly. A common symptom of brain inflammation is brain fog. If your entire body is inflamed or if you have an unmanaged autoimmune condition such as Hashimoto’s hypothyroidism, it is very possible your brain is also inflamed.
Another way chronic stress promotes brain degeneration is by constricting blood vessels and blood flow, depriving the brain of sufficient oxygen. Improved circulation is a necessary benefit of better managing Hashimoto’s hypothyroidism.
The best way to address stress is to cut unnecessary stressors from your lifestyle. It’s also important to address lesser known factors that are still very stressful, such as poor diet, unstable blood sugar, inflammation, food intolerances, or poor circulation. These are also the foundations to managing Hashimoto’s hypothyroidism.
Stress is your body’s way of trying to warn you that you’re in danger and putting your well being at risk. Ask my office for ways to mitigate the effects of stress on your health and wellness and to manage your Hashimoto’s hypothyroidism.
July 27, 2015
How to keep your gut healthy while traveling abroad

Nothing refreshes the mental landscape better than an exciting trip to a foreign land. However, nothing can have you regretting that adventure more than being glued to the toilet with traveler’s diarrhea or vomiting instead of traipsing through temples and markets.
With some advance planning and knowledge about gut health, stomach bugs, and supplements that can protect your gut, you may be able to breeze through your trip without days-long sessions in the hotel bathroom.
Nix stomach bugs with hydrochloric acid
Hydrochloric acid (HCl) is the acid in the stomach. You can also obtain it in a supplement. Why would you want to take an acid when it seems everyone is taking antacids? Because it’s our first line of defense against stomach bugs and can help prevent traveler’s diarrhea.
It may surprise you to know that many adults are deficient in HCl, especially the ones who suffer from acid reflux and pop antacids. This is because if stomach acid is low, food in the stomach is improperly digested. This lack of acidity also fails to trigger the valves that usher the food into the intestines. As a result, it ferments in the stomach, causing that burning feeling, and then shoots back up into the esophagus, scalding its delicate tissue. Although antacids bring relief, they fail to address the problem of low stomach acid.
HCl is vital to not only digest food, but also to kill bacteria, yeast, and other harmful pathogens. When stomach acid is low, you are more vulnerable to stomach bugs. Throw in strange, new cuisine of questionable hygiene in a developing country and you’ve got yourself an impending date with the porcelain god. Or the hole in the bathroom floor.
The best way to avoid this is to take HCl supplements with your meals. It’s best to begin this regimen before your trip so you can acclimate your digestive system to the change in chemistry and dial in your dose. Keep upping the dose with each meal until you feel burning. Then go back to the previous dose. As your natural acidity improves, you may find you need less over time. However, while traveling, it’s a good idea to take HCl prophylactically to lower the risk of traveler’s diarrhea.
Probiotics outwit bad bugs by beefing up the good bugs
Another great digestive force to support is your own colony of beneficial gut bacteria. A slew of research in recent years has established how vital the three to four pounds of gut bacteria in our intestines are to our mental, immune, and digestive health.
It’s hard to say whether popping a probiotic only during your travels will have much preventive measure of traveler’s diarrhea. But if you start beefing up the good bugs several months prior, you’ll head into uncharted culinary territory better fortified. One of the best ways to nourish your good bacteria is to make vegetable a primary part of every meal, even breakfast. Add cultured foods and drinks to your diet (such as kefir and kimchi), and boost your colonies with probiotic supplements. You may also need an herbal cleanse of the harmful bacteria to “weed the inner garden.” Ask my office for advice on how to do that.
Best prevention to traveler’s diarrhea is a healthy gut
The best way to lower your risk of traveler’s diarrhea is to start your travels with a healthy intestinal environment before your journey. This includes making sure you have sufficient stomach acid, repairing leaky gut, cleansing out overgrowths of bad bacteria and yeasts, and eating a whole foods diet that is primarily vegetables while avoiding sweets, processed foods, and restaurant foods. Ask my office for more info on preventing traveler’s diarrhea.
July 20, 2015
If you have autoimmunity you need to look at leaky gut
One of the primary things we look for when someone has autoimmunity is leaky gut, a condition in which the intestinal wall is damaged, as it is usually a key factor. Autoimmunity is an extremely common disorder today in which the immune system attacks and destroys part of the body. Common autoimmune disorders include Hashimoto’s hypothyroidism, type 1 diabetes, rheumatoid arthritis, psoriasis, celiac disease, multiple sclerosis, and vitiligo. However, there are many more.
What is leaky gut?
Leaky gut, a condition in which inflammation damages the intestinal wall and makes it overly porous, creates a hyper inflammatory state in the body that can predispose one to autoimmunity. Also known as intestinal permeability, it has been shown to play a role in triggering and exacerbating autoimmunity.
Leaky gut is still a relatively new concept. Science once believed the digestive system’s only role was to digest foods and absorb nutrients. Now we know it also serves as barrier between the outside world and the inside of the body, and that it is home base to the immune system.
When you consistently eat foods that are inflammatory (junk foods, sugars, foods to which you are sensitive), are exposed to infectious yeast and bacteria, live with constant stress, take certain medications, or drink too much alcohol, the integrity of the gut and the immune system breaks down. As a result, the immune system becomes hyper zealous and can begin to attack the body, creating autoimmunity.
Repairing leaky gut can help improve autoimmunity
Now that researchers have established the role of leaky gut in autoimmunity, they suggest we can slow down the autoimmune process or even send it into remission by repairing a leaky gut wall. Repairing leaky gut prevents undigested foods and other foreign invaders from escaping into the bloodstream where they trigger the immune system. When you are dealing with autoimmunity, you do not want to give the immune system a reason to be activated unnecessarily. If every meal and snack you eat contains a food that activates your immune system, you are keeping inflammation alive. An anti-inflammatory diet and repairing leaky gut are key to managing your autoimmune condition.
Symptoms of leaky gut
Obvious symptoms of leaky gut are digestive symptoms, including bloating, gas, constipation or diarrhea, and food sensitivities.
However, many people with leaky gut have no gut symptoms. Instead, they may have problems with their joints, skin, lungs, mood, brain function, or fatigue, depending on how inflammation affects that person.
When autoimmunity causes leaky gut
Sometimes autoimmunity itself causes leaky gut as it creates chronic inflammation that can damage the gut wall. This is particularly true in the case of autoimmunity to gut tissue, which may cause symptoms of irritable bowel syndrome. In these cases it’s especially important to follow a leaky gut diet and to focus on nutritional compounds that dampen inflammation. Ask my office for more information.
Mystery symptoms? It could be an autoimmune reaction
Do you have chronic, mysterious symptoms that drag your life down but your lab tests come back normal? You may have an autoimmune reaction, a disorder in which your immune system attacks and destroys a part of your body.
Autoimmunity can strike any tissue or compound in the body and symptoms will vary based on the part of the body attacked. However, people with autoimmunity have many symptoms in common:
- Extreme fatigue
- Muscle weakness
- Swollen Glands
- Inflammation
- Allergies
- Digestive problems
- Memory problems
- Headaches
- Low-grade fevers
Medicine has yet to fully recognize autoimmunity
Identifying autoimmunity can bring considerable relief. It validates you are not lazy, crazy, or that it’s all in your head, as many people struggling with autoimmunity feel.
Autoimmunity has exploded in incidence in recent years and neither medicine nor society fully accepts it unless it is at its most severe, end stages. Autoimmunity can slowly undermine your health and quality of life for years of decades before it is medically recognized.
This leaves those with autoimmunity alone in their struggle, wondering what’s wrong and why no one will acknowledge their suffering. Identifying autoimmunity with proper testing provides solid proof for the fatigue that keeps you pinned to the couch, chronic pain, unexplainable weight gain or loss, depression, poor brain function, and other symptoms.
Testing for autoimmunity
You can identify autoimmunity by screening for antibodies against a particular tissue with a blood test. Antibodies are proteins made by the immune system that attach to the affected tissue to tag it for destruction. You can screen for antibodies to thyroid tissue, joint tissue, brain tissue, the pancreas, and other tissues in the body.
For instance, the book Why Do I Still Have Thyroid Symptoms? talks about screening for Hashimoto’s, an autoimmune thyroid disease, by running antibodies against thyroid peroxidase (TPO), the enzyme that is a catalyst for thyroid hormone production, and thyroglobulin (TGB), a protein involved in thyroid hormone production. If those come back positive then you know autoimmunity is responsible for weight gain, depression, fatigue, constipation, cold hands and feet, and more.
Screening for individual autoimmune reactions is difficult and costly and conventional medicine does not offer treatments to manage autoimmunity until it is in more severe stages. This is why doctors don’t screen for it more routinely. Also, many types of autoimmunity are still considered obscure. The average doctor will not think to test for autoimmunity the brain, the adrenal glands, the ovaries, or bladder muscle, even though these autoimmune disorders are more common than people realize.
Modern, comprehensive testing for autoimmunity
Fortunately, we now have a lab test called the Array 5 Multiple Autoimmune Reactivity Screen through Cyrex Labs, that screens for antibodies to 24 different tissues at once much more affordably than running them individually. It can help both the patient and practitioner understand what is causing symptoms.
A positive (or equivocal) response indicates the immune system is tagging that particular tissue for destruction. However, it’s important to know that a positive result does not necessarily mean you have autoimmune disease. It could indicate your body is in the early stage of autoimmunity, which may be silent or causing less severe symptoms. By following autoimmune management protocols you may be able to keep it in a silent or less severe stage indefinitely.
The Cyrex Array 5 panel screens for the following antibodies to indicate specific autoimmune reactions:
- Parietal cell and ATPase instrinsic factor: stomach autoimmunity
- ASCA, ANCA, and tropomyosin: intestinal autoimmunity
- Thyroglobulin and thyroid peroxidase: thyroid autoimmunity
- 21 hydroxylase (adrenal cortex): adrenal autoimmunity
- Myocardial peptide, alpha-myosin: cardiac autoimmunity
- Phospholipid platelet glycoprotein: phospholipid autoimmunity
- Ovary/Testes: reproductive organ autoimmunity
- Fibulin, collagen complex, arthritic peptide: joint autoimmunity
- Osteocyte: bone autoimmunity
- Cytochrome P450 (hepatocyte): liver autoimmunity
- Insulin, islet cell, glutamic acid decarboxylase (GAD): pancreatic autoimmunity
- GAD, myelin basic protein, asialoganglioside, alpha and beta tubulin, cerebellar, synapsin: neurological autoimmunity
To learn more about your chronic symptoms of how to manage your autoimmunity, contact my office.
Finally! FDA initiates ban on partially hydrogenated oil

The FDA already requires food manufacturers to list the amount of trans fats in their products. It also removed trans fats from the category of Generally Recognized as Safe (GRAS).
However, now the FDA is working to remove partially hydrogenated oils from the food supply.
Food manufacturers have three years to phase them out of use, which should make boxed, packaged, and restaurant foods safer.
FDA banning trans fats to protect heart health
The FDA cites heart disease risks for banning trans fats. Trans fats contribute to a build up of plaque in arteries and increase the risk of heart disease. The FDA says removing trans fats from the food supply will prevent thousands of fatal heart attacks each year.
Trans fats also shrink the brain
Partially hydrogenated oils also shrink the brain and increase the risk of dementia. One study found that even very small amounts of trans fats damage the brain.
This is important to know because manufacturers are not required to list trans fats on the nutrition label if they contain less than 0.5 grams of trans fat per serving. If you see partially hydrogenated oil listed in the ingredients, then avoid that food (even if the nutrition label says 0 grams trans fat).
Hydrogenated oils are closer in structure to plastic than food and damage the brain in more than one way. They deprive the brain of oxygen by clogging arteries that bring blood to the brain.
They also become part of brain cell membranes. Cell membranes, which are comprised of fats, communicate with other cells and determine what enters and exits the cell. When hydrogenated oils in the diet become part of cell membranes, this makes them more rigid and less functional. The sheaths that insulate and protect neurons also incorporate trans fats.
This process also replaces the vital brain fats DHA and essential omega-3 fatty acid. As a result, cellular communication suffers, brain tissue degenerates, and disorders such as poor mental performance, mood disorders, memory loss, or health problems can arise.
Avoiding trans fats
Always read ingredient labels and ask food servers what type of oil is used for frying. Here are foods that commonly contain hydrogenated oils:
- Crackers, cookies, cakes, frozen pies and other baked goods
- Snack foods (such as some microwave popcorn)
- Stick margarines
- Coffee creamers
- Refrigerated dough products (such as biscuits and cinnamon rolls)
- Ready-to-use frostings
Brain-friendly diet
Ditch trans fats and go for a brain-friendly diet that includes leafy green vegetables, seafood, eggs, olive oil, nuts, avocados, colorful fruits, nuts, and meats.
To learn more about ways to eat for healthier brain function, check out the leaky gut/autoimmune diet and ask my office for information.
Goodbye McDonald’s; hello to healthier eating
McDonald’s is
In response to falling sales, McDonald’s is investigating dumping antibiotic-laced chicken and rBST (hormone) milks, adding sirloin burgers, and even introducing kale smoothies and salads.
Although we still have a long way to go as a nation, consumer habits point to an increasing consciousness of healthier eating. No doubt many of the 36 percent of Americans who are obese would rather not be, and are cutting back on fast food consumption as a result.
New technology helping Americans live healthier
Health experts also point to the increased use of smart phone apps and the rising popularity of health tracking technology, such as the FitBit, for cajoling Americans to become more interested in their diets.
For instance, some apps let you use your smart phone to scan product bar codes for nutrition information. Other apps make logging your diet and exercise easy — awareness is fundamental to healthier habits.
Apps also can plug you into a community of others on the same path to make you more accountable, to seek and offer support, and to share victories. One app (Pact) even requires a financial commitment: If you don’t meet your goals you have to pay up, and if you do, you earn money from those who haven’t.
Eating and living healthier requires simple changes
Avoiding McDonald’s and eating more healthfully doesn’t have to be a burden. It just requires simple steps. Also, unless a chronic illness requires immediate remediation, lasting dietary and lifestyle changes are best taken on bit by bit.
With that said, here are some steps you can implement to join the growing ranks of healthy eaters.
Educate yourself
Why are you eating healthier? Do you understand how it will improve your health? Even a little bit of self-education is hugely empowering and motivating.
Plan your meals
Eating at McDonald’s is often a stressed-out, last-minute decision. Healthier eating requires advance planning, such as packing food or knowing where to eat out. For instance, it’s not as cheap, but health food stores such as Whole Foods can offer much healthier and still very quick meal options.
Make a grocery list
Take some time to think about your grocery list. Do some research, explore, try new things. It can make healthier eating fun.
Clear out the old temptations
Empty your house of all the junk foods so you don’t fall into bad habits. Find some new, healthier treats for those times you need a comfort food.
Cook in batches
Healthier eating requires more preparation and cooking. You can save time by chopping and storing veggies ahead of time, or cooking large meals and freezing serving sized portions for later.
June 22, 2015
Poor sleep habits linked with dementia

Do you have trouble falling asleep? Do you fall asleep around 2 or 3 a.m. and sleep until noon? Or do you wake up at 4 a.m. and can’t fall back asleep?
Studies show insomnia does more than make the days drag — it raises your risk of dementia later in life. Heart disease, diabetes, obesity, mood disturbances, constipation, prostate cancer, and breast cancer have all been linked with poor sleep. Poor sleep is a growing problem, as is dementia. Twenty percent of the population is estimated to sleep too little (less than 6 hours a night). Insomnia is the most common sleep disorder today, affecting 64 million people, and one in three people over 65 will die of dementia.
Researchers found a particularly strong link between poor rapid eye movement (REM) sleep and dementia. These people do not go into the deep enough REM sleep that induces paralysis. Instead, they have vivid, violent dreams that they act out through punching, kicking, screaming, and even jumping out of bed. Sixty-three percent of people with this REM disorder develop dementia or Parkinson’s later in life.
The sleep wake cycle and dementia risk
Our circadian rhythm regulates our sleep/wake cycles — when we feel tired at night and alert in the morning. A healthy circadian rhythm is tied to daylight and darkness and governs sleeping and waking.
However, when this sleep/wake cycle becomes overly imbalanced, your risk of developing dementia, Alzheimer’s, and other diseases increases.
This is because the area of the brain that governs the circadian rhythm, the hippocampus, also plays a role in short-term memory and learning. The hippocampus is the first area of the brain to degenerate in dementia and Alzheimer’s disease.
Constant problems with your cycles of sleeping and waking could point to problems in the hippocampus and an increased risk of dementia later in life.
The sleep-wake and dementia
Researchers have found the risk of dementia was higher in older women with weak circadian rhythms, and tracking circadian rhythms over time has been shown to predict cognitive decline in older adults.
Are you at risk for dementia later in life?
How do you know if your circadian rhythm is off balance? Look at whether you suffer from any of the following symptoms:
- Difficulty falling asleep or staying asleep
- Difficulty waking in the morning
- Not feeling rested after sleep
- Poor recovery from exercise
- Drop of energy between 4 –7 p.m.
Preventing dementia by supporting sleep
Fortunately, there are steps you can take to better regulate your circadian rhythm and lower the risk for dementia. A primary tactic is to regulate cortisol, an adrenal stress hormone. Studies show high cortisol from constant physical or mental stress degenerates the hippocampus.
Stress isn’t just a lifestyle issue. Stress is also be caused by blood sugar swings, inflammation, food intolerances, hormone imbalances, and other metabolic issues. Inflammation in particular is associated with degeneration of the hippocampus. High homocysteine on a blood panel, a telltale sign of inflammation, is one way to determine whether inflammation is undermining your brain health.
Inflammation and dementia
A primary way to normalize the circadian rhythm and reduce your risk of dementia is to reduce inflammation. Your diet is the first places to start. This includes removing foods to which you are sensitive (gluten and dairy are among the more common), stabilizing your blood sugar, and eliminating processed foods.
Ask us about an anti-inflammatory diet, improving sleep, and other tools to lower the risk of dementia.
June 15, 2015
Worried about losing your memory? Eat your greens

Memory loss and dementia are valid concerns for everyone these days: one in three seniors dies of Alzheimer’s or dementia and Alzheimer’s is the sixth leading cause of death in the United States. Fortunately, dementia is largely preventable with many lifestyle and dietary adjustments, one of which is including plenty of greens in your diet.
New research shows eating plenty of spinach, kale, collards, and mustard greens can help slow cognitive decline. Researchers believe the high vitamin K content in these vegetables plays a role in preserving brain health.
The study tracked almost 1,000 older adults during five years and saw significantly less cognitive decline in participants who ate leafy green vegetables.
In fact, the elders who ate one to two servings a day of leafy greens had the cognitive ability of someone 11 years younger.
Researchers credited not only the vitamin K in leafy greens for slowing cognitive decline, but also lutein and beta-carotene. Other brightly colored fruits and vegetables are also high in these vitamins.
Vitamins aren’t the only brain benefits of leafy greens — greens promote healthy gut bacteria
The vitamins in leafy greens aren’t their only benefits.
For one, leafy greens are also rich in fiber, which are good for the gut. Plenty of dietary fiber not only prevents constipation, but it also supports the healthy bacteria in your gut. People who eat diets high in plant fiber show a more beneficial composition of gut bacteria compared to those who eat a typical western diet.
Scientists have increasingly been discovering how vital beneficial gut bacteria are to brain health. For instance, healthy gut bacteria promote the integrity of the blood-brain barrier, the lining that protects the brain.
Gut bacteria have also been shown to influence depression, anxiety, learning, and memory. This is because the gut and the brain communicate closely with one another through the vagus nerve, a large nerve that runs between the brain and the organs.
Eating greens is usually part of a healthy brain lifestyle
Another factor to consider with this study is that people who eat greens every day are typically more conscious of their health. Someone who is taking the time to shop for and prepare greens every day is probably eating a healthier, whole foods diet and avoiding dementia-promoting junk foods, sodas, and sugars.
Exercise is the golden bullet to lasting brain health
People who eat healthier also tend to exercise more regularly, whether it’s just taking a daily walk or hitting the gym every day. Both strength training and aerobic exercise have been shown protect neuron health, ensure better blood flow to the brain, and protect the brain from the damaging proteins that cause Alzheimer’s.
One study that followed more than 600 people ages 70 and older found those who engaged in the most physical activity showed the least amount of brain shrinkage.
Another study found that older adults who walked as little as 30 to 45 minutes three days a week increased the volume of the part of the brain responsible for learning and memory.
So although eating your greens is a great way to boost brain health (and gut health), if you eat your greens AND exercise every day, you drastically reduce your chances of developing dementia and Alzheimer’s. Considering there is no cure for dementia and Alzheimer’s — the neurons that die in these conditions cannot be recovered — the best approach is a preventive one.
Ask my office for more details on lowering your risk of dementia and Alzheimer’s.
June 08, 2015
Fight causes of allergies when you have Hashimoto’s

The end of winter seems like a good thing until your allergies go haywire. If you’re tired of allergy meds and always feeling stuffed up and zonked out, consider lasting relief by healing your gut to balance your immune system. The good news is that if you have Hashimoto’s hypothyroidism, the same approaches will help you better manage your thyroid condition.
It’s hard to believe your digestive tract can affect your sinuses, but both systems are similar as they serve as the body’s defense from the outside world. Plus, the digestive tract serves as a hub for the immune system. When you’ve got allergies, it’s worth investigating gut health. The same goes with Hashimoto’s hypothyroidism.
One of the most common links to allergies is leaky gut, also known as intestinal permeability. Leaky gut is like it sounds — the lining of the small intestine becomes inflamed, damaged, and leaky, allowing undigested foods, bacteria, yeasts, and other toxins into the bloodstream.
Whenever this happens, which can be with every meal, the immune system attacks these invaders. This causes inflammation and an over zealous immune state that plays a role in triggering or exacerbating seasonal allergies and autoimmune disorders such as Hashimoto’s.
Some people get seasonal allergies, but others get other inflammatory disorders, such as joint pain, skin problems, digestive complaints, autoimmune diseases such as Hashimoto’s hypothyroidism, issues with brain function, fatigue, chronic pain, and more.
How do you know if you have leaky gut? Sometimes you don’t, as you may not have any digestive complaints.
For some, leaky gut can cause bloating, heartburn, gas, constipation, diarrhea, or pain. Others see a link between leaky gut and skin problems, joint pain, brain fog, or sinus symptoms and allergies. For instance, some people notice when they eat certain foods they get brain fog, a runny nose, aching joints, or other immune issues. You should always investigate leaky gut if you have seasonal allergies and Hashimoto’s hypothyroidism.
Causes of leaky gut
Chronic stress, certain medications, and excessive alcohol consumption can cause leaky gut.
One of the most common causes of leaky gut is gluten. For some people, a gluten-free diet allows the gut to heal, thus profoundly relieving allergy symptoms. Gluten has also been linked in studies with Hashimoto’s.
Because leaky gut leads to food intolerances and food allergies, many people need to eliminate other foods, such as dairy, eggs, soy, or other grains. Many allergy sufferers have found significant relief following an anti-inflammatory diet. You can also ask my office about a lab test to screen for food sensitivities.
Imbalanced gut bacteria and seasonal allergies
We all have three to four pounds of bacteria in our digestive tract. These bacteria profoundly influence immune health, digestive health, and even respiratory and sinus health. After all, the sinuses and respiratory tract are lined with bacteria, too. Poor diet and lifestyle stressors can cause too many bad bacteria to grow, crowding out the good bacteria and setting the stage for infection, leaky gut, and autoimmune diseases such as Hashimoto’s. Probiotics and fermented foods can help populate your system with healthy bacteria.
Fix your allergies by fixing your gut
Leaky gut repair is based primarily on diet and lifestyle changes. Avoid processed foods, junk foods, sugars, and other industrialized foods. In other words, stick to a simple whole foods diet with plenty of vegetables (they nourish your good gut bacteria).
Certain supplements and nutritional compounds can help soothe and repair the lining of the digestive tract and calm inflammation in the sinuses and respiratory system.
Seasonal allergies are a red flag that your body needs care and attention. By addressing the underlying causes of your seasonal allergies you may also prevent the development of more serious conditions, such as autoimmune disease, depression, anxiety, or neurological disease.
Ask my office for more information on addressing the underlying causes of your seasonal allergies and Hashimoto’s hypothyroidism.
May 29, 2015
Hashimoto’s and autoimmunity linked to autism

Managing your hypothyroidism isn’t just about losing weight and having warm hands and feet. If you’re a woman who could get pregnant, it could play a role in whether you have a child with autism. A 2015 Finnish study that looked at risk factors associated with autism found that women who tested positive for autoimmune hypothyroidism, or Hashimoto’s, were more 80 percent more likely to give birth to a child who developed autism than women who did not.
Hashimoto’s is an autoimmune condition in which the immune system destroys the thyroid. But Hashimoto’s is only one of many autoimmune diseases. Autoimmunity means the body’s immune system attacks and destroys the very thing it was designed to protect — you. Which organ, gland, tissue, or chemical the immune system attacks depends on different factors, such as genetic predisposition and what triggered the autoimmunity. For instance, certain foods or chemicals are linked with certain autoimmune conditions. Rates of autoimmune disease are skyrocketing and many people go undiagnosed for years or a lifetime despite symptoms.
Similar studies have also made correlations between autoimmune diseases in the mother and increased risk of autism in their offspring. For instance, celiac disease, type 1 diabetes, and inflammatory bowel conditions have also been suggested as links to autism.
Why maternal autoimmunity can cause autism
Why can maternal autoimmunity cause autism in a child? Immune cells, called antibodies, that coordinate attack of the mother’s body in autoimmunity can be passed to the child. This can cause the child to be born with an autoimmune reaction already taking place in his or her body. In some case of autism, they are finding that these children are born with autoimmune attacks happening in the brain.
Evidence of this was demonstrated in a startling way when scientists injected one group of pregnant monkeys with antibodies taken from human mothers with autistic children. Another group of pregnant monkeys was injected with antibodies taken from mothers of neurotypical children. Compared to the control group, the monkeys who received the antibodies from mothers of autistic children gave birth to monkeys who grew to demonstrate atypical social behavior.
Manage autoimmunity before pregnancy
If you’re a woman who would like to get pregnant, it’s important to screen for and appropriately manage any autoimmune condition you may have. For instance, if you have Hashimoto’s hypothyroidism, it’s not enough to just take thyroid hormone. If you leave the autoimmune component of your thyroid condition unchecked, it could lead to more autoimmune diseases and you are at risk of passing the autoimmune antibodies to your child.
Managing autoimmunity is a comprehensive dietary and lifestyle approach designed to regulate an overzealous immune system so it does not attack the body. People with unchecked autoimmunity tend to be in very inflammatory states. Autoimmune management involves a comprehensive diet to reduce this inflammation.
Sometimes chemicals or metals can trigger or exacerbate autoimmunity, so it’s good to screen for that as well with the Cyrex Array 11 Chemical Immune Reactivity Screen. This doesn’t tell you the quantity of chemicals or metals in your body like other tests, but rather whether your immune system is reacting to them. This is vital information when you have autoimmunity.
Lifestyle factors such as chronic stress, too little sleep, an unhealthy relationship, a job you hate, and other negative influences can also raise inflammation and provoke autoimmunity. These are important factors to consider as well when managing an autoimmune disease.
It’s vital to shore up your health, balance your immune system, and manage any known or undiagnosed autoimmune reactions before getting pregnant to increase the likelihood of having a healthy child. Ask my office for more pre-conception advice.
May 22, 2015
Fitness, not fatness, predicts longevity with Hashimoto’s hypothyroidism

We’ve long been told if we want to be healthier and live longer we need to drop the pounds, but turns out being fit is the best predictor for longevity, even if you’re overweight. This is good news for those who have long struggled with Hashimoto’s hypothyroidism and may not be able to reach their ideal weight. Staying regularly physically active, even if it’s just walking, is one of the best things you can do for your health.
A team of researchers examined a collection of studies that together looked at thousands of people for as long as 16 years.
They divided study subjects into three groups: normal weight, overweight, and obese. They then divided them into fit and unfit groups based on endurance tests, typically running on a treadmill.
Their analysis showed that the subjects’ performance in the endurance tests determined their mortality risk in the coming years, not their weight. In fact, the unfit people had twice the risk of dying as the fit people, regardless of their weight. Overweight and obese people who were fit had the same mortality risks as fit participants who were normal weight.
In a nutshell: A thin unfit person is twice as likely to die as an obese fit person. This is great news to those who have struggled much of their lives, unsuccessfully, to lose weight. As long as they keep exercising, they can expect to live a longer, healthier life.
A big downside to the study was that the majority of subjects were men, so we can’t say for sure how the results apply to women. Also, it would be interesting to look at a study like this in relation to diabetes, cancer, high blood pressure, Hashimoto’s hypothyroidism, and other chronic health risks. The researchers only looked at length of life and not occurrence of disease.
So what does being fit look like if you have Hashimoto’s hypothyroidism?
Fortunately, enjoying these benefits of being fit does not require you to be a warrior at the gym or at Crossfit. In fact, in functional medicine we know that over exercising (which varies from person to person) is a great way to tax your health. If you are working to manage your Hashimoto’s hypothyroidism, exercising excessively may work against you and cause your symptoms to worsen. It’s important to exercise in a way that is appropriate for your health.
Most of the “fit” study participants were evaluated for an average of eight to 12 minutes on a treadmill. This falls in line with federal guidelines that suggest as little as two and a half hours of exercise a week, which can be done in increments as short as 10 minutes at a time, qualify you as fit.
Ways to meet those weekly goals can include parking far enough away from your destination that you have to walk 10 minutes to reach it, using a standing or stationary bike desk at work, and taking regular brisk walks.
People with Hashimoto’s hypothyroidism may find they benefit from adding in regular walks, swims, and bike rides.
Exercise is about much more than living longer when you have Hashimoto’s hypothyroidism
The promise of a longer life does not actually provide much motivation for many people, especially those who are younger. Instead, it’s important to look at other benefits of regular exercise, such as better managing your Hashimoto’s hypothyroidism.
Regular walking and other exercise have been shown to improve brain function, ward off depression, and boost self-esteem, and even curb cravings and addiction.
May 20, 2015
FDA sued over gluten in meds; Hashimoto’s warning

Although about 1 percent of the population suffers from celiac disease, vastly more have gluten sensitivity and must also abstain from eating wheat to avoid a variety of health conditions that typically involve inflammation, such as Hashimoto’s hypothyroidism, joint pain, brain-based disorders, skin problems, gut problems, and more.
People with Hashimoto’s hypothyroidism should be careful to avoid gluten as several studies and countless patient anecdotes have shown a link between gluten sensitivity and Hashimoto’s hypothyroidism.
The man sued the FDA after they failed to respond to a petition he filed after developing gluten reactions to a generic drug he had been taking.
Manufacturers do not disclose the use of wheat in their prescription and OTC drugs, making it a crapshoot for those with celiac disease or gluten sensitivity who must take them. The man filing the lawsuit had to call the manufacturer to inquire about the use of gluten in that specific batch of drugs. (Filler ingredients are changed regularly.) Although it’s unclear how many drugs contain gluten — a serious problem when it’s that difficult to ascertain — a university pharmacist has so far catalogued 150 drugs that don't contain gluten. Unfortunately, however, even these drugs are questionable as there is no oversight regarding cross-contamination with gluten. In other words, if the drugs are made on equipment or in an area contaminated with gluten, then they are no longer gluten-free. Many drugs also contain corn, potato, or soy, ingredients that may cross-react with gluten, causing symptoms.
It’s good to know which drugs contain gluten, especially since some autoimmune diseases such as Hashimoto’s hypothyroidism are linked in the science with gluten. If you take a medication regularly to help manage your autoimmune condition (such as insulin), it’s worth calling the manufacturer to ensure it is gluten-free. Gluten is linked to 55 diseases so far, the majority of them autoimmune and neurological.
Gluten also in many household products; exercise caution when you have Hashimoto’s hypothyroidism
Medications aren’t the only thing not required to list gluten as an ingredient. Some body products and household items also contain gluten. When you have Hashimoto’s it pays to be careful about using gluten on your body.
Manufacturers often use wheat in fillers, lubricants or absorbents in various body products. While gluten is not absorbed through the skin, it is possible to transfer traces from your hands or face to your mouth, where it can be swallowed and cause symptoms.
Examples of products that may contain hidden gluten include cosmetics and lip balm; lotions and sunscreens; stickers, stamps, and envelope glue; toothpaste; soaps; play dough; pet food; and laundry detergent.
When you have Hashimoto’s hypothyroidism it pays to be careful with your body and household products to avoid an inflammatory reaction.
How to protect yourself from hidden gluten when you have Hashimoto’s hypothyroidism
Unfortunately, your doctor or pharmacist may not know whether a drug or product contains gluten. It may be up to you to hunt down which are safe. The list of gluten-free drugs compiled by the university pharmacist is helpful.
Fortunately, when it comes to body and household products, many people have already done the research and reported their results online. Finding out whether a product is safe may be just a click away so you don’t have to go through the hassle of tracking down the right person in the company.
In response to consumer demand, an increasing number of companies are making and marketing gluten-free body products so just a quick glance at the label can tell you if it’s safe for you when you have Hashimoto’s hypothyroidism.
Also, finding safe play dough for kids can be a hassle; the name-brand stuff is wheat-based and we know it’s difficult for kids to keep their hands out of their mouths. Fortunately, some gluten-free brands of play dough are now available online, as well as plenty of very easy recipes to make your own.
Although it takes a little bit of extra effort to use medications and other products that are gluten-free, it’s worth the peace of mind to avoid provoking inflammatory reactions and symptoms.
May 8, 2015
Fight causes of allergies when you have Hashimoto’s

It’s hard to believe your digestive tract can affect your sinuses, but both systems are similar as they serve as the body’s defense from the outside world. Plus, the digestive tract serves as a hub for the immune system. When you’ve got allergies, it’s worth investigating gut health. The same goes with Hashimoto’s hypothyroidism.
One of the most common links to allergies is leaky gut, also known as intestinal permeability. Leaky gut is like it sounds — the lining of the small intestine becomes inflamed, damaged, and leaky, allowing undigested foods, bacteria, yeasts, and other toxins into the bloodstream.
Whenever this happens, which can be with every meal, the immune system attacks these invaders. This causes inflammation and an over zealous immune state that plays a role in triggering or exacerbating seasonal allergies and autoimmune disorders such as Hashimoto’s.
Some people get seasonal allergies, but others get other inflammatory disorders, such as joint pain, skin problems, digestive complaints, autoimmune diseases such as Hashimoto’s hypothyroidism, issues with brain function, fatigue, chronic pain, and more.
How do you know if you have leaky gut? Sometimes you don’t, as you may not have any digestive complaints.
For some, leaky gut can cause bloating, heartburn, gas, constipation, diarrhea, or pain. Others see a link between leaky gut and skin problems, joint pain, brain fog, or sinus symptoms and allergies. For instance, some people notice when they eat certain foods they get brain fog, a runny nose, aching joints, or other immune issues. You should always investigate leaky gut if you have seasonal allergies and Hashimoto’s hypothyroidism.
Causes of leaky gut
Chronic stress, certain medications, and excessive alcohol consumption can cause leaky gut.
One of the most common causes of leaky gut is gluten. For some people, a gluten-free diet allows the gut to heal, thus profoundly relieving allergy symptoms. Gluten has also been linked in studies with Hashimoto’s.
Because leaky gut leads to food intolerances and food allergies, many people need to eliminate other foods, such as dairy, eggs, soy, or other grains. Many allergy sufferers have found significant relief following an anti-inflammatory diet. You can also ask my office about a lab test to screen for food sensitivities.
Imbalanced gut bacteria and seasonal allergies
We all have three to four pounds of bacteria in our digestive tract. These bacteria profoundly influence immune health, digestive health, and even respiratory and sinus health. After all, the sinuses and respiratory tract are lined with bacteria, too. Poor diet and lifestyle stressors can cause too many bad bacteria to grow, crowding out the good bacteria and setting the stage for infection, leaky gut, and autoimmune diseases such as Hashimoto’s. Probiotics and fermented foods can help populate your system with healthy bacteria.
Fix your allergies by fixing your gut
Leaky gut repair is based primarily on diet and lifestyle changes. Avoid processed foods, junk foods, sugars, and other industrialized foods. In other words, stick to a simple whole foods diet with plenty of vegetables (they nourish your good gut bacteria).
Certain supplements and nutritional compounds can help soothe and repair the lining of the digestive tract and calm inflammation in the sinuses and respiratory system.
Seasonal allergies are a red flag that your body needs care and attention. By addressing the underlying causes of your seasonal allergies you may also prevent the development of more serious conditions, such as autoimmune disease, depression, anxiety, or neurological disease.
Ask my office for more information on addressing the underlying causes of your seasonal allergies and Hashimoto’s hypothyroidism.
April 7, 2015
SIBO common cause of wasting away in elderly

Symptoms of SIBO
For most people, symptoms of SIBO are straightforward. One of the most common symptoms is bloating after eating, particularly after eating grains, desserts, or other starchy foods. Other SIBO symptoms include gas, belching, indigestion, heartburn, nausea, abdominal pain and cramping, and either constipation, diarrhea, or both.
Doctors often misdiagnose SIBO as irritable bowel syndrome (IBS), as the symptoms are so similar. In fact, SIBO has been found in more than 80 percent of patients diagnosed with IBS.
Wasting away in elderly is usually SIBO symptom
Most doctors and patients haven’t heard of SIBO and blame this rapid decline in the elderly on aging. However, researchers have identified SIBO, which is treatable, as the leading cause of malabsorption, and thus wasting away, in older adults.
SIBO doesn’t always result in malabsorption and wasting away. People can fall anywhere along a range of symptoms, from asymptomatic to the severe. But those who fall in the middle of the spectrum can become progressively worse. That’s why complaints of bloating and gas after meals should be taken seriously and not thought of as normal.
As SIBO and malabsorption worsen, nutrition status can plummet. Levels of B vitamins drop, which impacts many functions in the body, including brain function. Inflammation may also increase as the body’s ability to regulate immune function deteriorates. It seems no matter how much older people with SIBO supplement, they cannot improve their low vitamin D status or persistent anemia.
The most devastating consequence of untreated SIBO and malabsorption is that it profoundly affects brain health and function, increasing the risk of dementia. It also saps energy and vitality. When an older person complains of bloating and distention after meals, it should not be dismissed as a minor complaint but rather taken seriously as a red flag indicating more serious problems down the road.
The cause and treatment of SIBO
A variety of things can cause SIBO, including antibiotic use, poor diet, and digestive damage, such as from a long-standing undiagnosed celiac condition.
In older adults (and in those who have sustained a concussion or brain injury), another cause to watch out for is declining brain function. The digestive tract depends on healthy brain function to work properly. When signals from the brain to the gut are not robust enough, the ileocecal valve, which separates the large intestine from the small intestine, may weaken and allow contents from the large intestine to travel backward into the small intestine, where they colonize. It is not the bacteria themselves that cause SIBO symptoms, but the byproducts they produce. These bacteria also compete with the host for protein in the diet.
Treatment for SIBO includes a strict diet to starve the bacteria, as well as targeted botanicals to kill them. Doing specific exercises to improve communication between the brain and the gut can also help prevent SIBO from perpetuating.
April 1, 2015
Do you sometimes “crash” with debilitating fatigue?

In fact, a recent survey of almost 8,000 autoimmune patients found the overwhelming majority listed bouts of debilitating fatigue as one of their most troubling symptoms.
Any number of things can cause a person with autoimmunity to “crash.” They can include a very stressful event, such as a car accident or a move. Pleasant events can cause crashes because they are long or exhausting, such as a wedding, a trip out of town, or a work conference. Many people hold up fine during the event but crash when it’s over. Exposure to certain foods or chemicals causes it in others.
Because such crashes are not commonplace or medically recognized, they cause anxiety and embarrassment. It’s like having the flu or a bad cold, except without the symptoms. Sufferers worry others will think they are lazy, another stressor on top of stressing about all the things not getting done because you’re in bed, barely able to function. Unfortunately, brain power bottoms out along with physical energy, which makes working at home from your laptop difficult if not impossible.
New survey brings light to autoimmune crashes
Fortunately, you may not have to make excuses for your inability to function forever as awareness about these bouts of debilitating fatigue grows. The survey polled those suffering from a variety of autoimmune diseases, such as Hashimoto’s hypothyroidism, rheumatoid arthritis, celiac disease, or autoimmunity affecting the brain or nervous system.
Overwhelming number of autoimmune patients report debilitating fatigue
The survey of patients with autoimmune disease, which was conducted by a patient advocacy group, revealed:
- 98 percent suffer from fatigue
- 89 percent said fatigue was a major issue
- 59 percent said fatigue was their most debilitating symptom
- Two-thirds said their fatigue was profound and prevented them from doing everyday tasks
- 75 percent said fatigue impacts their ability to work, 40 percent said it causes financial stress, and another one in five said it has cost them their jobs and they’re on disability
- The overwhelming majority reported fatigue not only impacts their professional life, but also their romantic and family life and self-esteem.
- The overwhelming majority also say it has resulted in emotional distress, isolation, anxiety, and depression.
According to one patient, “It’s difficult for other people to understand fatigue when it can’t be seen. It’s hard trying to get others, even doctors, to understand how very tired you are. One wonders if they think we are just mental cases or whiners.”
Fortunately, using functional medicine approaches can significantly improve your health and reduce the frequency and severity of these bouts of fatigue. Ask my office for more information.
March 24, 2015
Daylight Saving Time can be hard with Hashimoto’s

DST doesn’t just make people tired in the morning. Studies show the number of car accidents increases after DST, likely due to tired drivers. A Swedish study also found that the risk of heart attacks goes up the first few days after DST, and that risk drops after setting the time back to Standard Time. An Australian study showed an increase in suicides the first few weeks after DST goes into effect.
Some people aren’t ruffled by the change in time, others recover in a few days, and then there are those for whom DST means a few weeks of feeling out of whack while their body adjusts. In fact, one study showed our bodies never fully adjust to DST until we switch back to Standard Time. Night owls are affected the worst, taking as long as three weeks to recover. Research has shown on their days off, people revert to sleeping and waking according to what’s seasonally appropriate, not what DST dictates.
We are designed to gradually adjust to the changes in light as the seasons change. Forcing this change overnight once a year flies in the face of our internal clocks, which are tuned into nature.
This is because light dictates how much of the sleep hormone melatonin we make. The more light we are exposed to the less melatonin we make so that we are awake longer.
The sudden disruption to our internal clocks with the time change and loss of sleep causes a loss in production, concentration, and memory, as well as fatigue and sleepiness during the day.
When you are working to improve your Hashimoto’s, the change in time can set you back in your healing journey.
DST bad for business as well as Hashimoto’s
DST isn’t just hard on health for those who have Hashimoto’s. Enacted during World War I to decrease energy costs, DST has now been shown to actually increase energy demands, due largely to more air conditioner use and more driving time to daylight activities. Also, contrary to popular belief, it does not benefit farmers; they actually oppose it. Dairy farmers in particular say cows do not easily adapt to the change in schedule. Orthodox religions don’t like their sunrise and sunset prayer tinkered with. However, the golf, barbecue, and retail industries love it. Broader research has shown DST costs the economy anywhere from $400 million to $2 billion due to loss of productivity, workplace injury, and “cyber loafing.”
How to cope with Daylight Saving Time
If DST is wrecking you and flaring your Hashimoto’s symptoms those first few weeks, you can do a few things to help ease the transition (in addition to signing an online petition to end DST):
Lay low until you adjust. Honor the disruption to your natural rhythms and take it easy by avoiding taking on extra activities or added stressors until you feel back to normal. Also, avoid dangerous activities.
Add in extra time to rest and nap. The biggest cost of DST is sleep loss, especially if you are a night owl. It is difficult to go to bed and wake up an hour earlier. Make time for a nap or at least some time to lie down and rest during the day those first few weeks.
Block blue light at night to help you adjust. Wearing orange glasses in the evening a couple of hours before bed will also help increase the production of sleep hormones so you can fall asleep. Exposure to sunlight during the day will also help regulate sleep hormones. You can use a light box in the mornings to help you wake up.
Ask my office for advice on helping you sleep better and managing your Hashimoto’s.
March 17, 2015
The problem with perfumes when you have Hashimoto’s

Perfumes contain chemicals derived from petroleum that have been associated with hormone disruption, allergic reactions, cancer, birth defects, nervous-system disorders, and a tendency to accumulate in human tissues, although most haven’t been tested for safety at all. For instance, some are linked to sperm damage and are found concentrated in human fat tissue and in breast milk. About 3,000 chemicals fall under this category, however manufacturers are simply required to label them as “fragrance.” These toxic effects can make it more difficult to manage Hashimoto’s hypothyroidism.
In fact, 75 percent of products that list “fragrance” as an ingredient contain phthalates, a chemical linked to cancers, hormone disruption, and neurological disorders. Although many countries have banned phthalates and the U.S. has banned them in toys, they continue to be used in perfumes, including those marketed to children.
Unfortunately, you can buy organic foods, drink filtered water, use non-toxic products, and run an air purifier in your home, but you can’t escape perfume scents. They’re in your neighbor’s dryer sheets venting next door, other people wear fragrances or use them in their homes, they’re in air fresheners and insecticides in public buildings, in soaps in public restrooms, and so on. If you participate in public life, you are exposed to synthetic scents. As for your own product use, if you see “fragrance” on the label, then you know it contains an indeterminate amount of these chemicals. You should avoid these products if you have Hashimoto’s.
How to reduce the risk of developing a chemical sensitivity to perfumes when you have Hashimoto’s
Some people have lost their tolerance to chemicals and exposure to perfumes, dryer sheets, scented detergents and so on can trigger any number of symptoms, including migraines, incontinence, fatigue, inflammation, or a worsening of an autoimmune condition. For instance, someone with multiple sclerosis, an autoimmune disease, who is sensitive to chemicals may lose muscle control of her legs when exposed to perfume. Or if it may worsen your Hashimoto’s symptoms.
Here’s how you can reduce your risk of developing a sensitivity to perfumes and other synthetic chemicals:
- Reduce the toxic burden on your body. This means not using products in your home or on your body that contain synthetic chemicals. Also, avoid foods that have artificial colorings and additives, which also have been linked to numerous health disorders.
- Make sure your glutathione status is good. Glutathione is the body’s master antioxidant that defends your cells against toxic chemicals. By reducing your toxic burden you protect your glutathione stores. You can also take supplements to boost glutathione production. Ask my office for details.
- Remove foods to which you are sensitive. If you regularly eat a food to which you have an immune sensitivity, such as gluten, it causes your immune system to be hyperactive and more prone to developing sensitivities to other things, such as chemicals. Do a food immune reaction panel from Cyrex Labs or an elimination/provocation diet to find out which foods trigger inflammation in you.
These tips are also vital to managing Hashimoto’s.
You don’t have to give up wonderful scents, simply switch to essential oils and natural scents. Some essential oils not only smell good but they are therapeutic as well. However, those with a sensitivity to perfumes may not be able to tolerate natural scents.
March 2, 2015
Avoid food coloring when you have Hashimoto’s

What do Europeans know that we don’t? Actually, they have access to the same science we do, only apparently they take it more seriously. The good news is that, thanks to pressure from consumers in the know, food giant Nestle is leading the way by voluntarily removing food dyes from its chocolate candies by the end of 2015.
So what’s the big deal with food coloring? Are the risks for real or is it just a bunch of hype?
Immunologist Aristo Vojdani, PhD, outlines the various health risks and disorders associated with food colorings in one of his many published papers, and in his upcoming book, When Food Turns Against You.
Following is a list of ways artificial food colorings have been found to be harmful. If you have Hashimoto’s hypothyroidism please avoid worsening your condition by avoiding artificial food colors:
- Food coloring is linked to hyperactivity and ADHD. This is one of the most commonly known health consequences associated with food dyes.
- The caramel coloring used in soft drinks has been found to pose a cancer risk.
- Many people, children especially, consume far more food coloring than has been measured for safety. A bowl of colored cereal exceeds the amount of food coloring that has been found to cause behavioral issues in some children.
- Artificial food coloring binds to proteins in foods it is added to. Human digestive enzymes cannot break down many of these proteins once they are bound to food coloring. This creates intestinal inflammation and damage, leading to leaky gut.
Food coloring also binds to human tissue and proteins in the blood. This is what turns kids’ lips and tongues bright colors after they eat a lollipop or snow cone. Human autopsies have revealed entire colons dyed blue or green due to food coloring. The problem is the immune system does not recognize human tissue once it is bound to food coloring and it may begin to attack the tissue. This can lead to permanent autoimmunity to that organ or tissue. Also, once these colors are bound to cells in the body, those cells cannot function properly.
- Food coloring causes allergic reactions in some people, causing a runny nose, hives, welts, and neurological reactions.
- Food coloring can lead to a breakdown in oral tolerance, or the ability of the immune system to tell friend from foe. This can result in increased food and chemical sensitivities.
These are just some of the ways artificial food colorings, which are made from petroleum, adversely affect human health. Although food manufacturers prefer artificial colors over natural ones because they mix easily, are cheaper, and more stable, they are just not worth the cost to your health, especially if you are trying to manage Hashimoto’s hypothyroidism.
Food dyes are not just in obvious things such as candies and sodas. They lurk in salad dressings, pickles, crackers, meats (particularly tandoori chicken), desserts, medications, soaps, cosmetics, lotions, toothpastes, and other products.
A vitally important step as you transition to a whole foods diet to manage your Hashimoto’s hypothyroidism is to eliminate all artificial colorings and other additives from your diet and from the products you use on your body.
Journey through the gut – the Hashimoto’s gut guide

“All disease begins in the gut,” said Hippocrates. Understanding digestion helps you understand why you stay well or get sick.
From north to south — the Hashimoto’s guide
Because so much of the immune system resides in the gut, a healthy digestive tract is paramount to managing Hashimoto’s.
Good digestion starts in the brain. When your brain gets the message you’re about to eat, it turns on the “rest and digest” part of the nervous system to prepare the organs. When we eat while distracted, busy, or anxious our saliva won’t be as rich in digestive enzymes, our stomach won’t be sufficiently acidic, and our pancreas will not secrete enough digestive juices.
The mouth and the stomach — important for thyroid health
The majority of our digestion takes place in the mouth, where, ideally, we chew each bite thoroughly, allowing the enzyme-rich saliva to begin breaking down our food, signaling the nervous system to rest and digest, and alerting the rest of the digestive tract that it’s time to work.
Next stop is the stomach, which uses its powerful muscles to further mash the food while liquefying it with hydrochloric acid (HCl). The proper acidity digests the food for optimal nutrient absorption; sterilizes it by killing bacteria and other pathogens; and alerts the small intestine to open the pyloric valve and allow it in. Once there, the pancreas secretes enzymes and the gallbladder secretes bile to further digest the food.
Unfortunately, about 90 percent of Americans are deficient in stomach HCl due to stress, poor nutrition, bacterial overgrowth, poor thyroid function, and advancing age.
When the stomach environment is not acidic enough, the small intestine is not triggered to allow the food in, so it sits in the stomach, where it begins to ferment and putrefy. Eventually it may shoot back up into the esophagus, burning the tender tissue there and causing heartburn, or acid reflux.
This breakdown is the first step to causing poor gut health that can trigger or exacerbate conditions such as Hashimoto’s.
The small intestine
Eventually the small intestine must accept the fermenting food. Because it is not the right acidity, the pancreas and gallbladder are not sufficiently triggered to release enzymes and bile.
This is problematic for several reasons: Improperly digested fat irritates the rest of the digestive tract; nutrient absorption is poor, and an inactive gallbladder is more prone to forming gallstones. Because it is the avenue through which the liver excretes toxins, a congested gallbladder results in a congested, overburdened liver unable to detoxify the blood properly.
As this rotting mess makes its way through the intestines, it causes inflammation and damage that leads to intestinal permeability, or “leaky gut.” Leaky gut allows undigested food proteins to escape into the bloodstream, where the immune system attacks them, causing inflammation. Because undigested foods are the target of attack, food intolerances and autoimmune diseases such as Hashimoto’s develop.
The colon
Our colons host 3 to 4 pounds of friendly bacteria, or gut flora. These bacteria break down foods and produce nutrients. However, breakdowns further north foster an overgrowth of bad bacteria, causing an inflamed, poorly functioning colon.
New research is showing gut flora play an important role in virtually all aspects of health, including in thyroid health and autoimmunity. A healthy balance of gut bacteria is vital to managing Hashimoto’s.
Hashimoto’s hypothyroidism can begin in the gut
Although general gut health is vital to managing Hashimoto’s hypothyroidism, it’s also important to note that about 20 percent of thyroid hormones are converted to the active form you’re body is able to use in the gut. If you suffer from poor gut health, your body may not be getting enough of the thyroid hormone it needs for optimal function.
While various drugs offer quick fixes for digestive complaints, they allow us to ignore the red flags the gastrointestinal tract is waving to gain our attention. Poor digestion underlies just about every disease known to man, including Hashimoto’s in many cases. This is a topic to which functional medicine practitioners devote their careers.
Ask my office how we can better support your gut health and manage your Hashimoto’s hypothyroidism.
February 16, 2015
Suffering from burn out? Look at Adrenal Health

Unfortunately, the adrenal glands are under siege by our stressed-out modern lives. In addition to stress, blood sugar swings, gut infections, food intolerances, chronic viruses, environmental toxins, and autoimmune conditions tax the adrenal glands. The body interprets all of these as threats, causing the adrenal glands to pump out stress hormones to raise blood sugar to meet the demands of the stress. What should be an occasional mechanism is a daily thing for most.
Symptoms of adrenal stress include fatigue, weak immunity, allergies, low blood sugar, being groggy in the mornings, crashing in the afternoon, sleep problems, and more.
Adrenal imbalances are one the most common health problems we see in functional medicine thanks to high-stress lifestyles, high-carb diets, and a toxic environment.
Adrenal problems always secondary to something else
Adrenal health is always secondary to something else. Blood sugar imbalances are a very common cause of adrenal problems. The adrenal hormone cortisol raises blood sugar when it drops too low, which, when it happens repeatedly, exhausts the adrenal glands, as well as the brain’s control center over these functions. Constant cortisol production weakens the lining of the intestines tract, making it more susceptible to bad bacteria, inflammation, and leaky gut.
Other factors that can contribute to adrenal problems include autoimmune disease, food intolerances, chronic infection, chemical sensitivities, and hormonal imbalances.
Lab tests to assess adrenal health
We can measure adrenal function with a salivary panel. The most important thing to know about the panel is that one test is not worth much. It is the follow-up test that shows whether a protocol is improving your health. If it’s not, we dig deeper.
You take the test kit home and collect samples of your saliva in the morning, at noon, in the afternoon, and at bedtime to measure cortisol at each time. It should be highest in the morning so you feel alert and lowest at night so you feel tired for bed. This is called your circadian rhythm, or sleep-wake cycle. Chronic stress eventually disrupts the circadian rhythm. An abnormal circadian rhythm can cause high cortisol at night and insomnia, or low cortisol in the morning, which makes it hard to wake up.
Adrenal problems can cause hormone problems
When adrenal stress is high, the body steals a hormone called pregnenolone from cholesterol to make more cortisol — a phenomenon known as pregnenolone steal. Normally, the body uses pregnenolone to make sex hormones such as progesterone and testosterone. As a result, pregnenolone steal causes hormonal imbalances such as PMS, infertility, male menopause, and polycystic ovary syndrome (PCOS).
Avoid Adrenal Stimulators
If you are serious about restoring your adrenal health, avoid the things that tax it, such as sugar, caffeine, nicotine, alcohol, foods to which are you sensitive, lack of sleep, over exercising, over working, bad relationships, and other stressors.
Stabilize blood sugar to support adrenals
Stabilizing blood sugar is paramount to supporting the adrenals. This is especially true for those with low blood sugar who get irritable, shaky, or lightheaded if they go too long without eating. Eat a protein breakfast and then eat small meals frequently to keep your blood sugar from crashing. Avoid relying on caffeine or sugar for energy, and do not skip meals.
Schedule relaxing things
Find ways to relieve stress and remain calm. Learn some relaxation techniques, take yoga, walk daily, take time off, socialize, and other things that support your well being in a positive and healthy way. Just knowing you have something fun and relaxing planned is half the battle to lowering stress.
Ask my office for help in supporting your adrenal health.

Aging people have long since been resigned to living out their latter years avoiding salt and eating a bland, tasteless diet. But new research shows the risks of salt may be overblown. Also, if you have low blood pressure, salt can actually serve as a boost to your health. It’s important to boost low blood pressure if you have Hashimoto’s as that will improve blood flow.
Salt has been recognized as a precious commodity throughout human history, even serving as a form of legal currency. Not only is it vital to our health, it also preserves foods and, as anyone who has accidentally cooked a meal without salt can attest, it is vital to making food taste good.
However, salt came to be overused in the industrialization of food. This led to concern over a link between increasing rates of high blood pressure and a higher rate of heart disease risk.
However, new research suggests we don’t have to abandon this ancient culinary delight. A study of almost 3,000 older people in their 70s found no significant risk for cardiovascular disease, heart failure, or death in those who consumed about a teaspoon of salt a day versus those who didn’t. Current health guidelines call for consuming no more than 1,500 mg of salt a day for those over 50, and 2,300 mg (about a teaspoon) for those under 50. The average American consumes almost 3,500 mg, thanks to our fast-food culture.
Of course, if you have high blood pressure, this is not license to eat lots of salt as that can worsen the situation. It’s important to also consider the role of potassium, which lessens the effects of salt. The recommended daily intake of potassium is 4,700 mg a day. Foods high in potassium include sweet potatoes, greens, bananas, citrus fruits, and more. Also, when it comes to blood pressure, other important factors are exercise and reducing sugar and carbohydrate intake if you have insulin resistance.
High blood pressure or not, it’s important not to over consume the heavily salted processed foods that contain chemically laden industrialized salt. These foods contain other harmful ingredients that will work against you if you are trying to manage Hashimoto’s hypothyroidism, including gluten, hydrogenated oils, and artificial additives.
Salt is beneficial if you have low blood pressure and Hashimoto’s hypothyroidism
Natural salt has benefits that include trace minerals and being free of chemical additives found in conventional salt. If you have low blood pressure, eating plenty of salt is especially important to boost blood flow to your tissues and brain. A blood pressure of 120/80 is considered healthy and if the upper or lower number deviates by 10 your blood pressure is in an abnormal range.
Low blood pressure is associated with adrenal fatigue. The adrenal glands produce stress hormones and help regulate blood pressure. Many people today have fatigued adrenal glands thanks to chronic stress, poor diets, chronic inflammation, and more. Symptoms of adrenal fatigue include constant tiredness, low blood sugar, and low blood pressure. Adrenal fatigue and low blood pressure are common in many people with Hashimoto’s hypothyroidism. If you don’t work to manage these conditions, it will be more difficult to manage your thyroid condition as well.
In addition to salt, certain nutritional compounds support adrenal function and thus healthy blood pressure. Ask my office for more information on how to support healthy blood pressure and Hashimoto’s hypothyroidism.
Could loneliness be the cause of addiction?
Addiction can apply to any substance or activity (alcohol, drugs, shopping, sex, food, gambling, Facebook, etc.) that delivers pleasure but becomes compulsive and interferes with daily life and health. The addict is often not aware his or her behavior is out of control. Addiction is recognized as being a reaction to emotional stress; loneliness is so stressful it carries the same mortality risk as smoking and is twice as dangerous as obesity. Our physiological aversion to loneliness stems from our days as hunters and gatherers, when connection with others improved the odds of survival.
Research shows loneliness impairs the brain’s ability to exercise control over our desires, emotions, and behaviors –- the sort of qualities necessary to maintain healthy habits and avoid bad ones. This is called having executive control, and without it, we are more susceptible to addictive behaviors. Loneliness also triggers our fight-or-flight stress hormones, further creating that need for relief that erodes willpower and propels addictive behavior.
Studies show social connection inhibits addiction In older studies on addiction, rats placed in cages with a bottle of pure water and a bottle of water laced with heroin or cocaine inevitably chose the drugged water until it killed them. The rats were alone.
However, rats kept in a comfortable cage with plenty of friends, fun activities and toys sampled the drug-laced water but mostly shunned it, consuming less than a quarter of the drugs the isolated rats consumed. Also, unlike the isolated rats who became heavy drug users, none of the socialized rats died.
After two months of addictive drug use, researchers then took the isolated rats and put them in the fun, socially active cages. The rats exhibited withdrawal symptoms initially and then voluntarily gave up their addiction, despite the availability of the drug-laced water.
Researchers saw similar outcomes in humans during the Vietnam War, during which about 20 percent of soldiers became addicted to heroin. Of those who returned home, about 95 percent simply stopped using heroin, presumably because they shifted from a “terrifying” cage to a safer, more comfortable one.
And although painkiller addiction has become a serious problem, the majority of people temporarily prescribed pain pills for an injury or surgery don’t become addicted, even after months of use. These examples show evidence that drug addiction is not just a chemical dependency.
The remedy for addiction is connection
With one of the worst drug problems in Europe, Portugal put these principles to test. It jettisoned the war on drugs and instead poured resources into reconnecting addicts with their own feelings, other people, and a feeling of purpose through job programs. A follow-up study showed the program reduced the use of injected drugs by 50 percent.
Humans are wired to connect and bond with one another. If we can’t bond with other people we bond with the source of our addiction. Nutritional therapy, supplemental support (amino acids in particular can positively influence brain chemistry), and other functional medicine strategies can encourage healthy brain behavior that reduces addictive tendencies. However, it’s vitally important to also address the psychological and spiritual underpinnings of addiction, which often include loneliness and isolation.
Got Hashimoto’s? Diet sodas can prevent weight loss

We’re increasingly learning about the trillions of bacteria that live in the gut, weighing in at 3 to 4 pounds, and the profound influence they have on human health and behavior. In addition to providing nutrients and aiding in the digestive process, gut bacteria also influence moods, behavior and mental health; immune function; energy levels; and how well we burn or store fat.
Our microbiome consists of beneficial and harmful bacteria. We carry a diverse array of bacteria –- hundreds of varieties –- and the proportions of these bacteria can play a role in how our body, brain, and even personality function. A healthy composition of bacteria is also vital to managing autoimmune diseases such as Hashimoto’s hypothyroidism.
Unfortunately, as promising as the idea of calorie-free drinks sound, they skew the balance of bacteria in the gut toward high blood sugar. This in turn promotes insulin resistance (pre-diabetes), fat storage, and chronic inflammation. In the study this phenomenon was referred to as glucose intolerance. Together these factors sabotage not only weight loss but also your ability to manage Hashimoto’s hypothyroidism.
Artificial sweeteners promote high blood sugar The study began by looking at groups of mice that were given plain water, water with sugar added, or water with an artificial sweetener added. After 10 weeks the groups given the artificial sweeteners consistently showed high blood sugar, regardless of whether the sweetener used was saccharine, aspartame, or sucralose. Even a group of mice given a high-fat diet and sugar water maintained healthy blood glucose levels while the group given a high-fat diet and artificial sweeteners did not. To further validate the findings, researchers transplanted fecal matter from the mice given artificial sweeteners into germ-free mice. The germ-free, too, developed glucose intolerance. When scientists gavethe affected mice antibiotics to kill the overgrowth of fat-promoting bacteria, their blood sugar normalized.
Studying artificial sweeteners in humans Of course, not everyone is going to be sold on the results of a study using mice. After all, we’re not mice. So the researchers ran the study on a small group of human volunteers, all of whom showed elevated blood sugar and alterations in their gut bacteria composition after just one week.
How to cultivate healthy gut bacteria and better manage Hashimoto’s hypothyroidism In addition to avoiding artificial sweeteners, there are other ways to cultivate your inner garden of gut flora to promote fat burning instead of weight gain. One of the best ways is to make vegetables the primary part of your diet, including cultured vegetables. Not only are they loaded with fiber, vitamins, and minerals, they promote and maintain good gut bacteria. At the same time, avoiding processed foods, sugars and sweeteners, and artificial additives will prevent the bad bacteria from taking over and exacerbating your Hashimoto’s hypothyroidism symptoms.
Ask my office for probiotic supplement recommendations to further enhance your good gut bacteria and for help in managing your Hashimoto’s hypothyroidism.
Where does fat go when you lose weight?

How you gain weight We gain weight when we eat more food than we need. Those excess carbohydrates and proteins are converted into triglycerides (compounds made up of carbon, hydrogen and oxygen), which are stored in lipid droplets inside fat cells. Losing weight requires breaking down those triglycerides to access their carbon. Making triglycerides is an energy demanding process. Do you ever feel sleepy after a high-carbohydrate meal, like a big plate of pasta, a bowl or rice, a large dessert, or maybe simply too much food? That tired feeling stems in part from the energy your body requires to make triglycerides that can be stored as fat. Other weight loss tips
Naturally, you want to avoid that sleepy feeling, not only because naps are inappropriate at your work desk, but also because you’re making fat! Try reducing the amount of carbohydrates you eat and/or the amount of food to avoid that fat-promoting sleepy feeling. If you still feel sleepy after eating a healthy meal of moderate portion size and sensible carbohydrate content, you may need nutritional support to address insulin resistance. Ask my office for advice – some nutrients and herbs are very effective at helping stabilize blood sugar. Regular exercise not only helps you breathe away excess fat, but it also better sensitizes and regulates cell function to be fat burning rather than fat promoting. The key to promoting fat burning is to keep your blood sugar stable by not overdoing carbohydrates or portion sizes and by keeping your body active. Ask my office for more advice on how to turn your body into a better fat burner.
Have Hashimoto’s and can’t sleep? Your phone, computer, tablet, and TV cause insomnia
January 14, 2015

Do you like to play a little Candy Crush or surf Facebook before bed? Or maybe you’re vegging out in front of your giant LED television or reading a novel on your iPad. Then when you turn the lights off you toss and turn frustratingly into the wee hours of the morning, glancing constantly at the bright blue numbers on your alarm clock just inches from your face. You’re not alone – Americans are alarmingly insomniatic and sleep-deprived these days. The CDC says insufficient sleep is a public health epidemic and research has established that the constant exposure to blue light from electronic devices is a major culprit. If you have Hashimoto’s hypothyroidism, this can further disrupt an already delicately balanced immune system and make managing Hashimoto’s more difficult.
How smart phones, computers, tablets, and TVs cause insomnia and wreck your health if you have Hashimoto’s hypothyroidism
The bad news is not only are these much-loved devices causing chronic insomnia, but also long-term health problems because of the blue light they emit. Our brains perceive blue light as daytime light, which suppresses melatonin, the sleep hormone. Melatonin also plays a role in immune function, and chronic melatonin suppression has been linked to a higher risk of prostate, colorectal and breast cancers. Chronic sleep deprivation is also linked to obesity, diabetes, chronic inflammation, and other metabolic disorders. For the person trying to manage Hashimoto’s hypothyroidism, this is another obstacle that can sabotage your success.
In the latest study that looked at the effects of these devices on sleep, one group of subjects read on an iPad for four hours before bed while the other group read from a printed book in dim light. After a week, the groups switched. In just five nights, the iPad group displayed reduced levels of melatonin, they took longer to fall asleep, and they spent less time in the restorative REM sleep. They also reported being sleepier and less alert in the morning, even after 8 hours of sleep, and showed disruption in their sleep-wake cycle.
Because blue-light emitting devices have such profound biological effects, the research team proposed they be subjected to the same safety evaluations as drugs. A sleep poll shows 95 percent of Americans uses some kind of light-emitting device at least a few nights a week before bed, making this a national concern. If you have Hashimoto’s hypothyroidism, it’s important you address this aspect of your life to support your immune health.
What to do to sleep better without totally unplugging when you have Hashimoto’s
The obvious answer to sleep better is to quit using blue-light emitting devices at nightfall. But for most Americans that’s simply asking too much. Luckily strategies exist to protect your melatonin production when you have Hashimoto’s hypothyroidism:
- Use the Kindle e-reader that does not have a backlit screen. Or just read a regular book.
- Put orange bulbs in your lamps that you use at night, especially next to your bed.
- The simplest way to protect yourself from blue light at night is to wear orange glasses. You can buy a cheap pair from Amazon or choose from more style options at Low Blue Lights.
- Install the f.lux app on your computer or Android phone (it won’t work for iPhones). This turns the light on your screen an orangeish-pink hue.
Ask my office for other ways to support healthy sleep and Hashimoto’s hypothyroidism.
Make the New Year more active if you have Hashi’s
January 7, 2015

Most of us are starting the New Year with resolutions to improve, but few changes will improve your life more than regular physical activity, even if you have Hashimoto’s hypothyroidism. However, starting an exercise habit can seem insurmountable to the chronically tired and sedentary. This article offers tips to get you motivated to begin and stick with regular physical activity suited to your fitness level.
First off, there’s more to exercise than just weight loss. Have you seen the significant difference between elderly people who exercise versus those who don’t? That’s because the organ that benefits most from exercise is your brain, and regular exercise will help keep you sharp and nimble well into your golden years.
As long as you don’t do overdo it, some kind of exerciser or physical activity will also help lower the inflammation associated with Hashimoto’s hypothyroidism and regulate your immune system. The endorphins released by getting your heart rate up are calming to an overactive immune system that flares autoimmunity.
However, exercise’s reputation as a health panacea is not sufficiently motivating for most. To be motivating exercise needs to be fun and doable. It should feel good, not painful.
Research shows that once they make exercise a “should,” people lose interest. Managing Hashimoto’s or some other health condition loses out to the solace found in a bag of chips and the latest episode of Nashville. Fear-based motivation, such as the health threats of high blood pressure or bone loss, are slightly more motivating but still fail many.
You have to make exercise fun to stick with it
Adding to the burden is that fact that Americans today are overly busy. Working one or more jobs, single parenting, schoolwork in the evenings… it all makes trips to the gym seem like an extravagant, unnecessary luxury. However, those who make the time find exercise actually improves productivity in the rest of their day, almost as if it is mysteriously creating more time. This is because of the enormous boost in brain function it delivers.
When people feel stretched to the limit, they will only fit in what feels absolutely necessary. Therefore, say research psychologists, you need to create a compelling reason to exercise. Figuring out how to make it fun and deliver that immediate endorphin high is one way. Another way is to keep it short but intense so you’re not burning up too much time.
Keep it short but intense
For instance, challenge your kids to a few running races or pushup challenges to get in some short bursts of high-intensity interval training (HIIT). HIIT has been lauded as quick and easy but highly “therapeutic” form of exercise. The beauty of it is you can tailor it to your fitness level with the only goal being you boost your heart rate, rest, and repeat.
Add in a social element
Another well-proven strategy is to exercise with friends or in a group. This kills two birds with one stone by also fitting in the extremely health-promoting activity of socialization.
Exercise while you work
You also might want to work exercise into normally sedentary habits of long hours at the computer or vegging in front of the TV. New research shows that sitting disease, which comes from sitting for long hours every day, is a silent killer no matter how well you eat or how often you exercise. It’s up there with smoking in terms of health risks and shortens your life span while dulling your mood. Sadly, quitting your job to frolic on the beach is not in the cards for most of us. Instead, many people have found they can work while walking on a treadmill, standing at a desk, or riding a stationary bike. You can buy an expensive treadmill desk or a cheaper attachment for a treadmill that will hold your laptop. A variety of standing desks are now available, and a stationary bike with a built-in workstation has received many good reviews. The key is to work against gravity while you’re on the computer or watching TV, as that has been shown to be necessary for the body and brain to stay healthy.
Walk
Never underestimate the power of a daily walk. It is the easiest and perhaps the most enjoyable form of exercise available. Walking regulates brain and immune function, making it a great addition to a Hashimoto’s management protocol.
Are xylitol and other sugar alcohols safe with Hashi’s?
December 23, 2014

America is on a never-ending quest to satisfy its sweet tooth without the health risks of sugar and other sweeteners. If you’re working to manage Hashimoto’s hypothyroidism, you probably know to avoid toxic artificial sweeteners such as sucralose and aspartame, but what about the more “natural” ones, such as xylitol, erythritol, and sorbitol? Although they’re found on the shelves of health food stores, it’s worth knowing a few things about these “natural” sweeteners.
The good news about xylitol, erythritol, and sorbitol when you have Hashimoto’s hypothyroidism
Xylitol, erythritol, and sorbitol are sugar alcohols that are either poorly digested or poorly absorbed, which means they impart fewer calories and are less likely to raise blood sugar. Although they haven’t been studied much compared to artificial sweeteners, research of xylitol shows no negative effects except for gastrointestinal distress, which dissipated in some subjects in time. In fact, studies of diabetic rats showed xylitol improved health.
Xylitol is most well known for the prevention of tooth decay, better than fluoride in some studies. Sugar alcohols also do not appear to confuse the body and raise blood sugar in the way artificial sweeteners do.
The bad news about xylitol, erythritol, and sorbitol about Hashimoto’s hypothyroidism
The downfall of sugar alcohols is that they can wreak havoc on digestive health and comfort. Because sugar alcohols are largely indigestible they pull water into the digestive tract and can cause diarrhea. Also, their indigestibility can cause them to ferment in the gut, causing bloating, gas, and distention. However, some people are able to adjust in a month or two and symptoms dissipate. Of the sugar alcohols, erythritol is the most easily digested and therefore causes the least gastric distress.
You probably need to keep sugar alcohols off the menu if you have small intestinal bacterial overgrowth (SIBO), irritable bowel syndrome (IBS), Crohn’s, or other digestive problems. It may also be a poor choice if you are on the autoimmune diet to repair your leaky gut or manage your autoimmunity.
People who are on the FODMAPS (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) diet also need to avoid xylitol, erythritol, and other sugar alcohols. This diet helps many people living with chronic gastric distress find relief by avoiding foods that are poorly digested and ferment in the gut.
Using xylitol, erythritol, and sorbitol in your diet
If you’re trying to cut back on sugar and sugar alcohols don't upset your stomach, you may find them a way to add some sweetness without the blood sugar spikes and consequent metabolic breakdowns that occur from eating sugars and other sweeteners regularly. However, they are not as sweet as sugar with a much milder sweetness. If you use too much to try and compensate you could be left with an unpleasant aftertaste. These sugars still have calories and carbohydrates, so if eaten in excess they can sabotage your efforts to improve your health by cutting back on sweets. You should also know that they are often derived from corn, much of which is genetically modified in the US, and an allergen for many.
The best way around fake sugars is to grow accustomed to a healthy, whole foods diet that only includes sweeteners on occasion. When you do not eat sweets regularly you begin to lose your taste for them, and you find a piece of fruit enormously satisfying and plenty sweet. A healthy diet low in sweeteners and void of foods that worsen gut health is also important to manage Hashimoto’s hypothyroidism.
Try this to fall back asleep at 3 a.m. if you have Hashimoto’s
December 3, 2014

Do you have Hashimoto’s hypothyroidism and often wake up at 3 a.m., your mind racing with thoughts, and you can’t fall back asleep? Try this crazy sounding but highly effective tip: Eat something! Make sure it’s not something sweet but instead something with protein and fat, such as nut butter, a bit of hard-boiled egg, or some meat. Make sure to keep some food next to your bed with a glass of water so you don’t wake yourself up too much by going to the kitchen. You won’t feel hungry and most likely won’t feel like eating, but do it anyway as an experiment. Chances are you will fall right back to sleep. Why?
If things go according to plan you don’t bolt awake at 3 a.m. While you’re sound asleep you’re brain is hard at work and needs plenty of fuel. It is forming memories, clearing out old cells, regenerating — all while you’re fasting, having gone hours without eating. In order to give the brain the energy it needs, the body gradually raises cortisol, an adrenal hormone. Cortisol triggers the release or synthesis of glucose to fuel the brain during the nightlong fast and you sleep through the night.
That’s if things are working right. People with Hashimoto’s hypothyroidism often suffer from other metabolic disturbances, such as low blood sugar. If you suffer with chronically low blood sugar then you are one of those people who is likely to bolt awake at 3 or 4 a.m. People with low blood sugar will have difficulty making enough cortisol to sustain the brain during the night. To compensate and keep the brain going, the body then releases “fight-or-flight” adrenal hormones. These adrenal hormones raise blood sugar back to a safer level to give the brain fuel. Unfortunately, they also raise stress, which can cause anxiety or panic in the middle of the night. This explains why you wake up at 3 or 4 a.m. with a racing mind, an infinite to-do list, in a panic, or some other stress-addled state.
Things you can do during the day to avoid waking up at 3 a.m. if you have Hashimoto’s
Although a few bites of food may help you fall back asleep, it’s better to prevent that anxious wake up call in the first place. Managing your blood sugar is also paramount to better managing Hashimoto’s hypothyroidism. If low blood sugar has you waking up every morning at 3 try the following tips:
- Always eat breakfast, even if you don’t feel like it, and avoid sugary, high-carbohydrate foods with breakfast. Low blood sugar will cause you to wake up with no appetite. You may even feel nauseous. Eat anyway, you need to break the nightlong fast and stabilize your blood sugar.
- During the day eat frequently enough so blood sugar does not crash.
- Avoid sweets and starchy foods (breads, pasta, rice, potatoes, etc.) and adopt a lower-carbohydrate diet. People with low blood sugar symptoms typically eat too many sweets and starchy foods as well as frequently skip meals. Eat enough protein and healthy fats to sustain your energy.
Ask my office about nutritional compounds that can help you manage your blood sugar and sleep through the night. I can also help you better manage your Hashimoto’s hypothyroidism.
Get a candida infection under control naturally
What causes candida
Sugar. Candida can be caused by a variety of factors. The fungus thrives on sugar so diets high in sugars, processed carbohydrates, and alcohol feed allow a candida infection to take root and thrive. This also causes sugar cravings to increase to sustain its burgeoning population.
Antibiotics. Antibiotic use is another common cause. Although antibiotics kill off harmful bacteria, they also kill off the very beneficial bacteria in your intestinal tract that help keep candida from growing out of control. It’s important to reestablish healthy gut bacteria with probiotics or fermented foods after antibiotic use, and to avoid them whenever possible. Ask my office for advice.
Poor gut health. If you have gut problems you are more susceptible to a candida infection. If you are not able to digest your food properly, you have an imbalance between good and bad bacteria, your gut is inflamed, you have leaky gut, you suffer from chronic constipation or diarrhea, and other digestive disorders, you are more at risk for a candida infection. Candida is like a weed that grows best in a sickly, neglected garden.
Hormonal imbalances. Hormonal imbalances that affect women in particular can upset the balance of gut bacteria and gut health. For instance, too little or too much estrogen can contribute to a vaginal yeast infection as proper estrogen levels keep the vaginal tract more resistant to infection.
Poor circulation. If you have cold hands and feet or the tip of your nose is cold, this indicates poor circulation. Poor circulation makes you more susceptible to a candida infection because blood carries immune cells that fight fungus and other infections. When the blood does not fully penetrate into the tissues with these immune cells, tissues become more prone to infection. A common example is chronic nail fungus.
Low blood pressure is another culprit as the blood does not adequately push into body tissue.
Poor brain function from degeneration or past head trauma. One thing people don’t consider with a candida infection is brain function. If your brain is not functioning well due to a previous head trauma or because it is degenerating too quickly due to unmanaged health condition, you are at a higher risk for a candida infection. Why? Healthy brain function is necessary for a healthy gut — the brain and gut are in close communication with each other. The brain also regulates immune function and general health of the body. When the brain suffers the body suffers, leaving it more prone to a candida infection.
A candida infection is a warning symptom
A candida infection is a red flag warning you the body is out of balance. There are some very drastic candida diets on the Internet that seem designed more to provoke an eating disorder than cure a candida infection. You don't necessarily have to go to excessive extremes. A candida infection requires you to adopt a healthy, whole foods approach to eating that eliminates sugar, junk foods, and too many carbohydrates and to focus on plenty of leafy green vegetables, healthy meats, and lots of filtered water.
In addition to a good diet, a variety of herbs and nutritional supplements are highly effective at combatting a candida infection. You also need to remedy poor digestive health (this may require specific dietary modifications as well), boost brain function, or help balance hormones. Ask my office for advice.
Hashimoto's Thyroiditis Autoimmune Condition
September 19, 2014

Hashimoto's is the most common autoimmune condition. Most low thyroid patients actually have Hashimoto's. At LifeSpring Wellness Center in Bloomington Minnesota we focus on low thyroid. The problem most patients have when they get the medical diagnosis of hypothyroid or low thyroid is that they are given synthetic thyroid hormone called Synthroid or levothyroxine. Actually 80% of hypothyroid or low thyroid patients have an autoimmune problem, and find that only taking synthetic T4 does not help. Why? Because giving a hormone to someone who has an autoimmune problem does little if anything for their autoimmune, Hashimoto problem. We know that it is better to find out what is triggering the autoimmune response. Once we find the triggers and remove them, guess what? You start to feel better--that means more energy, better mood and joy in life, better focus and memory, and more comfort and aliveness. Dr. Gilman is a published thyroid researcher and has worked with low thyroid and low energy patients for over 30 years.
Low thyroid, hypothyroid affects brain function in Bloomington, MN
March 25, 2014
When you have low thyroid or hypothyroid, your brain does not get as much blood flow to it. This will cause fatigue in many. Also mood can be affected. That is often is experienced as depression and sadness. Low T3, which is a thyroid hormone can be a major factor in in sadness. At our clinic in Bloomington,MN we test our patients with symptoms of low thyroid or hypothyroid for many componenets of the thyroid hormones. We do tests like TSH, T4, free T4, T3, Free T3, Reverse T3, T3 uptake, TPO (for autoimmune, Hashimots's) and TG antibody (for TPO, Hashimoto's). Almost all patients who contact us that still have their hypothyroid or low thyroid symptoms, and are on medication. We find that most patients who have been diagnosed with low thyroid or hypothyroid have not had all the tests that I just mentioned. These added tests give us information as to why the medication does not work, and what to do to improve your energy, joy and focus. Once we do the added tests that have been missed, you can get your energy, joy and focus back. Life gets better.
Thursday, August 29, 2013
What is low thyroid dysfunction?
I get asked about low thyroid dysfunction often. Your thyroid system affects the production of energy in every cell of your body. It

Women with Low Thyroid August 1, 2013
Dr. Phil Gilman DC FMA, offers hope for women with low thyroid in Minnesota who have spent many years treating symptoms, yet still have their symptoms. Symptoms of low thyroid often have similar symptoms as other conditions, and the problem can be easily misdiagnosed. And, quite often, the basic medical tests such as TSH look “normal”, but you still don’t feel well. Traditional medical treatments won’t ultimately help the most common type of thyroid condition, which is Hashimoto’s disease. It’s important to find the cause of low thyroid, which usually is your immune system. Our process includes a customized approach to your situation with diet and nutritional supplements. We’ll monitor your progress and revise diet and supplements as needed to you reach your goal for a better quality of life.
Brain Based Therapy (Neuro metabolic therapy)
Neuro relates to Brain Based testing. This involves testing the cerebellum and cortex for imbalances. Metabolic testing involves lab tests and questionnaires to determine nutritional status, immune function, hormonal function like adrenal and thyroid. Without addressing both neurological and metabolic aspects it is difficult to help chronic problems.
Many chronic conditions such as MS, Restless leg syndrome, thyroid conditions, vertigo and balance problems, fibromyalgia and insomnia can be helped by identifying the functional problems.
Heart Disease
Presently, according to the American Heart Association, 1.3million coronary angioplasty and 448,000 coronary bypass operations are performed annually at a cost of more than $100 billion. Despite these costs, many studies, including one last month in The New England Journal of Medicine, reveal that angioplasties and stents do not prolong life or even prevent heart attacks in stable patients (ie. 95% of those who receive them6).
Coronary bypass surgery prolongs life <strong>in less than 2% to 3% of patients who receive it.
In contrast, the INTERHEART study, published in The Lancet in 2004, followed 30, 000 people and found that changing lifestyle <strong>could prevent at least 90% of all heart disease
Think about it. Heart disease accounts for more premature deaths and costs Americans more than any other illness and is almost completely preventable simply by changing diet and lifestyle.
The same lifestyle changes that can prevent or even reverse heart disease can prevent or reverse many other chronic diseases as well.
Medicare and insurance companies currently pay billions of dollars every year for surgical procedures such as angioplasties and bypass surgeries. These are high-risk, invasive, expensive procedures fraught with complications, and they are largely ineffective.
Diet, supplements, stress reduction, brain based therapy, chiropractic adjustments help restore balance. Checking thyroid, liver function, testing for gluten, and other factors are a good place to start.
If you are taking thyroid medication such as synthroid and still have thyroid symptoms it may because you have a different type of thyroid problem. There are many types of thyroid problems. For example your T4 must be converted to T3 in order to have effect. If your ability to convert T4 to T3 is faulty, then taking the synthetic form of T4 may not help you. After years of studying thyroid function and doing research I have found the answer to some of the resistant thyroid problems.
You need to figure out WHY there is poor conversion. Conversion occurs in the liver and gut.
There are functional tests to determine this problem! Yes it is possible to feel better!
Thyroid and cortisol
High levels of cortisol is hidden cause number five, why you still have thyroid symptoms even though you’re taking thyroid hormone or even though your lab numbers are normal.
Cortisol is a hormone made by your adrenal glands. Your adrenal glands sit on top of your kidneys. They make a lot of hormones for you...aldosterone, cortisol and androgens. You could say your adrenal glands are crucial for your good health.
Cortisol is the main thing that regulates your blood sugar--not insulin.
So follow me as I explain cortisol and low thyroid symptoms....
Your adrenal glands make cortisol in response to stress. There are different kinds of stress. Anything that promotes inflammation or that causes inflammation, will make your adrenal glands pump out more cortisol. As that cortisol is released, those cytokines are going to come out with it---that is what’s going to suppress your pituitary.
The most common causes of elevated cortisol are:
- Blood sugar regulation problems (high or low blood sugar, insulin spikes and valleys)
- hidden gut infections or infections you haven’t been able to eliminate
- chronic stress.
-->
Six tips for optimal sleep
Running around frantically just before slamming your head onto your pillow is not an effective way to achieve optimal sleep patterns for most people. Getting into a pattern of consistent, optimal sleep takes some time and can be greatly helped by following some basic sleep hygiene tips. Take a look at the list below and consider integrating a few into your routine for the next week to see if you can complete the following optimal-sleep challenge: Fall asleep within five minutes of lying down, sleep through the night without waking, and rise the next morning feeling rested and refreshed.
Find out why you do not sleep well.
1. Shut down your computer and turn off your cell phone and television 30 minutes prior to sleep. Create an environment that is quiet and calm.
2. Remove stimulants (television, stereo, computer, bright lights) from your sleeping area. Keep the bedroom clear from clutter -- remove any unnecessary furniture, piles of clothes, papers and books so things are kept out of sight and the space looks and feels calm and simple.
3. Make sure your sleeping area is as dark and quiet as possible. Consider a fan or other source of white noise to create a consistent environment.
4. Dab a drop of essential oil behind the ears. It should be a scent you've chosen only for sleep time, not something you might associate with your shampoo, dryer sheets, hand lotion, etc. The idea is to associate this scent with the sensation of feeling relaxed and tired.
5. Establish a set sleeping time and try your best to stick to it -- even if your work schedule requires that you work odd hours and even if that means you're sleeping each day from 1 a.m. to 9 a.m.
6. Find out WHY you have difficulty sleeping. For example, if you cannot fall asleep, you may have insulin resistance or hyper adrenals. If you cannot stay asleep you may have low blood sugar or adrenals. Are you waking up tired and with fatigue? Do you feel fatigue and get sleepy after noon lunch? Getting at the underlying cause is the most important factor. Blood sugar, adrenals, and thyroid problems could be causing your problem. We test to find that out for you. No guessing. Sound sleep is critical for health.
Just as we all need air, water and food to survive, we also need sleep to be healthy. By making optimal sleep a priority in your life, you may be amazed at the positive impact you can have on your mental and physical outlook. With a few simple rituals in place, and getting at the underlying cause, you lay the foundation for attaining optimal wellness.
Methyl groups are extremely important in liver detoxification, heart health, brain function, digestion of food, and normal function of most body functions. They even tell pregnant women to take their folic acid because of methylation.
Have you ever wondered WHY all of a sudden someone develops a neurodegenerative disorder, heart disease, an autoimmune condition or even...cancer?
Did it just drop down out of the sky.
No! They expressed a “bad gene!”
How do you express “bad genes” like autoimmune, MS, ALS, Parkinson’s, heart disease or cancer?
The answer is depleted methyl groups! Depletion of your body’s methyl groups is how “bad” genes are expressed.
How are methyl groups in our body depleted? By consuming a poor diet loaded with “white death”—white sugar, white flour, and white salt, “bad oils”—trans-fatty acids and hydrogenated oils, produce loaded with pesticides and herbicides, junk food, drinks loaded with caffeine, high-fructose corn syrup and acid, genetically-modified foods, and stress!
What helps create methyl groups?
HCL or stomach acid!
This is WHY it is vital for everyone to have the proper amount of stomach acid (HCL)!
We create massive amounts of HCL when we are young but as we age, we make less and less. Again, further decreases in stomach acid or HCL are caused by excess stress and a poor diet.
Methyl groups are VITAL for normal cell replication at the level of the DNA! They literally turn genes “on” or “off.”
When you have depleted methyl groups, bad genes like cancer causing oncogenes are turned “on” and good genes, like cancer preventing tumor-suppressor genes, are turned “off.”
When you have sufficient methyl groups, good genes, like tumor suppressor genes, are turned “on”, and bad genes, like oncogenes, are turned “off.”
Methyl groups are also vital for phase II liver detoxification, protein methylation, homocysteine metabolism (increasing the methyl groups decreases inflammation), neurotransmitter synthesis, and nucleic acid synthesis.
Inadequate methylation capacity can lead to birth defects, depression, cognitive decline, diseases and cancer. Impaired methylation has even been associated with autism.
So... a patient has depleted methyl groups and all of a sudden they come in contact with a toxin, prolonged exposure to EMFs, a dental infection, or severe emotional stress, and... BOOM... they express the bad gene. The next thing you know, they have a neurodegenerative disorder like Parkinson's, ALS, or Alzheimer's, they have an autoimmune condition, or they have cancer. None of these conditions drop out of the sky and land on a patient; there has to be a cause, and the cause is depleted methyl groups.
How do you test for adequate levels of HCL? By checking the patient’s blood work and looking at the total protein, serum globulin, BUN and phosphorus. If some or all are abnormal, you most likely have lower levels of HCL.
How do you test for methyl groups? There is a specific urine test that can be run called the Basic Organic Acid test. Make sure to contact Dr. Gilman at 952-300-2260 for more information.
IT IS NOT THE GENES, BUT WHAT WE EXPOSE THEM TO 2013-02-03
Despite common misconceptions, monogenic diseases, or diseases that result from errors in the
nucleotide sequence of a single gene are exceedingly rare. Perhaps only 1% of all diseases fall
within this category, and Celiac disease is not one of them. In fact, following the completion of
the Human Genome Project (HGP) in 2003 it is no longer accurate to say that our genes “cause”
disease, any more than it is accurate to say that DNA is sufficient to account for all the proteins
in our body. Despite initial expectations, the HGP revealed that there are only 30,000-35,000
genes in human DNA (genome), rather than the 100,000 + believed necessary to encode the
100,000 + proteins found in the human body (proteome).
The “blueprint” model of genetics: one gene → one protein → one cellular behavior, which was
once the holy grail of biology, has now been supplanted by a model of the cell where epigenetic
factors (literally: “beyond the control of the gene”) are primary in determining how DNA will be
interpreted, translated and expressed. A single gene can be used by the cell to express a multitude
of proteins and it is not the DNA itself that determines how or what genes will be
expressed. Rather, we must look to the epigenetic factors to understand what makes a liver cell
different from a skin cell or brain cell. All of these cells share the exact same 3 billion base pairs
that make up our DNA code, but it is the epigenetic factors, e.g. regulatory proteins and posttranslational modifications, that make the determination as to which genes to turn on and which
to silence, resulting in each cell’s unique phenotype. Moreover, epigenetic factors are directly
and indirectly influenced by the presence or absence of key nutrients in the diet, as well as
exposures to chemicals, pathogens and other environmental influences.
In a nutshell, what we eat and what we are exposed to in our environment directly affects
our DNA and its expression.
Within the scope of this new perspective even classical monogenic diseases like Cystic Fibrosis
(CF) can be viewed in a new, more promising light. In CF many of the adverse changes that
result from the defective expression of the Cystic Fibrosis Transmembrane Conductance
Regulator (CFTR) gene may be preventable or reversible, owing to the fact that the misfolding of
the CFTR gene product has been shown to undergo partial or full correction (in the rodent
model) when exposed to phytochemicals found in turmeric, cayenne, and soybean.
Moreover, nutritional deficiencies of seleniun, zinc, riboflavin, vitamin e, etc. in the womb or early in life, may “trigger” the faulty expression or folding patterns of the CFTR gene in Cystic Fibrosis
which might otherwise have avoided epigenetic activation.
This would explain why it is possible to live into one’s late seventies with this condition, as was the case
for Katherine Shores (1925-2004). The implications of these findings are rather extraordinary: epigenetic and not genetic factors are primary in determining disease outcome. Even if we exclude the possibility of reversing certain monogenic diseases, the basic lesson from the post-Genomic era is that we can’t blame our DNA for causing disease. Rather, it may have more to do with what we choose to expose our DNA to….
Summary:
Genes do not primarily directly cause disease.
Epigenetics causes will determine disease expression.
Epigenetic changes
- Chemical/Nutritional--- deficiencies and toxicities
- Thoughts---negative emotions/beliefs/stress events/unforgiveness
- Physical----trauma and lack of movement
